Dr. Bon Ku *09, wearing heavy-rimmed glasses, blue scrubs, and orange-and-black Air Jordans, hops onto a table that doesn’t look as if it was designed to hold the weight of an adult human. He lies face down on a cushion with three cutouts that supports his body from his head down to his hips. Ku is in the Health Design Lab he directs at Thomas Jefferson University in Philadelphia, demonstrating a simple option for treating hospitalized COVID-19 patients who need to be proned — carefully turned from their backs to their stomachs — to increase the oxygen level in their blood. Proning emerged as a strategy during the initial months of the pandemic, but for those patients who were conscious, especially those who were obese, it wasn’t always comfortable. Ku asked a fellow emergency-medicine physician in New York City for ideas, and the doctor mentioned prenatal massage pillows, with their deep indentations to accommodate a pregnant woman’s chest and belly. It’s an existing product with no bells and whistles, and it epitomizes one of Ku’s guiding principles: Design solutions don’t have to be high-tech or exciting. They just have to work.
Ku and his fellow members of the Health Design Lab (HDL) are approaching some of the questions raised by the novel coronavirus in the same way that they tackle other knotty problems in health care. They use design thinking, a human-centered, collaborative, creative mindset that begins with open-ended questions rather than a clearly defined hypothesis. A design challenge might begin with a big, sweeping question such as “How might we create fulfilling and sustainable roles for health-care providers?” or a narrower one, such as “How can a primary-care exam room be designed to improve a visit between a doctor and a patient?” And now, in the COVID era, there’s a whole new list of questions, such as “How might we design hospitals to protect their workers?” and “How might we expand widespread testing?”
Treating sticky problems as design challenges is the hallmark of the lab, which hosts collaborators from all over Jefferson and is the center of the design track at Jefferson’s Sidney Kimmel Medical College, one of seven “scholarly inquiry” tracks available to medical students. That design program is the first of its kind and is something like a minor for the 25 or so students per class who follow its curriculum throughout their four years of medical education. The work done at the HDL might result in a new device, process, program, or approach. The lab is “a test kitchen for the hospital,” says Ku. “We test new recipes for health care.” And like a test kitchen for food, some things end up on the menu, and others don’t. “Both are important,” he says.
Since late 2016, the lab has been located in a bank vault in the basement of an old Federal Reserve Bank building that was constructed in the 1930s and now houses Jefferson medical offices. Previously the space was “a graveyard for abandoned medicine equipment,” says Ku. When searching for a home for the lab, it was important that it be part of the hospital. “We wanted space for water-cooler moments,” where people from other departments could easily come to brainstorm and collaborate, he says. (It’s also an easy walk to and from the Jefferson emergency room, where Ku typically works two overnight shifts per week.) It’s about 4,000 square feet separated into two main sections: a large anteroom and a workspace. To get from one room to the other, you pass through an enormous round opening — the giant vault door now permanently propped open.
Since the pandemic hit, the layout has been reconfigured and equipment repurposed to focus on COVID-related projects. Masked lab members are using some of the lab’s 3D printers to make batches of what look like transparent swizzle sticks, but are actually single-piece nasopharyngeal swabs used to test for COVID infection. (The swabs, made out of surgical-grade resin, were designed at the University of South Florida; thanks to open-source computer files, they can now be manufactured at hospitals including Jefferson.) Lab members have also used the printers to produce “ear savers” that make the constant wearing of masks more comfortable.
At the same time, the lab is continuing to support non-COVID activities. One collaboration with surgeons began with a specific problem: During operations for head and neck cancers, surgeons needed to take precious time during the procedure to tailor to the patient the titanium plates used in reconstructing the jaw. How could they do that work earlier in the process? They turned to the HDL and its 3D printers. Now lab members use imaging data to print 3D models that help surgeons bend plates to fit the patient ahead of time. Because the printer uses scans converted to data files, the patient doesn’t even have to be on site. Those efforts have expanded to other surgeries. Ku and lab co-founder and managing director Robert Pugliese, an emergency-medicine clinical pharmacist by training, explain that caesarean sections on patients with uterine fibroid tumors are tricky because the benign tumors can hemorrhage if nicked by a scalpel. So the lab can now print 3D models of a patient’s uterus using MRI-scan data, showing the location, size, and shape of the tumors and permitting surgeons to better plan for the procedure.
Student projects have covered a range of health-care problems. One team of medical, occupational-therapy, and industrial-design students worked on improving the experience of pelvic exams — which can be unpleasant under the best of circumstances — in the ER. Because ERs typically lack gynecological beds, “clinicians often improvise by pushing a bedpan under the person’s pelvis,” wrote Ku and Ellen Lupton — a senior curator for contemporary design at Cooper Hewitt, Smithsonian Design Museum — in Health Design Thinking, a book published in March. That could be demeaning and lead to suboptimal exams, they wrote. To design an alternative, empathy for the patient was key. To better understand that patient perspective, two male med students got on a table and assumed the position necessary for a pelvic exam. Team members talked to hospital administrators to understand the constraints on cost and storage of a potential device. They eventually came up with a prototype: “a collapsible, portable wedge that is moderately priced, medically appropriate, and easy to store,” called Tilt, the book reports.

Ku aspired to medicine initially because it was his parents’ “American dream,” as he said in a 2016 TEDx talk. His mother and father immigrated from South Korea and worked at a variety of jobs around the U.S. before opening a restaurant in Newark, New Jersey. (They’re now retired in South Korea.) They wanted a career in medicine for their firstborn son. And so, Ku says, it became his dream, too. He went to the University of Pennsylvania, where he majored in classical studies and studied Greek and Latin, and then to Penn State for medical school. He disliked it — not because of the school itself, but because of medical education in general, which felt outdated given the complex world med students graduate into. “We’re training [students] to practice in the 20th century, and we need to change that to the 21st century,” he says. Ku longed for less memorization and more emphasis on creative thinking and problem-solving. But he was energized by the possibility of being able to immediately help another human being, something he’d witnessed on an undergraduate trip to El Salvador, where he watched physicians treating patients in a poor community. “The health needs of these patients were overwhelming to me, nothing like I’d ever encountered before,” he says.
Emergency medicine offered him the chance to give people the immediate help they needed, and Ku started at Jefferson in 2006. He enjoyed his job, and he pursued research in bedside ultrasound. But after a while, Ku had a creeping feeling that he wasn’t making a difference. In his 2016 TEDx talk, he said he felt as though he was keeping patients from dying, rather than helping them to live. He believed he wasn’t addressing the larger forces that were bringing people to his ER. He noticed that he was repeatedly seeing the same patients, mostly people of color from the most underserved Philadelphia neighborhoods, struggling to control chronic diseases like Type 2 diabetes. “What can I really do about this?” he wondered.
Seeking inspiration and time to think, Ku stepped away from the ER for a year and enrolled in the one-year master of public policy program at the Princeton School of Public and International Affairs. “It was a total reset,” he says. He took classes in various disciplines, learning from economist Uwe Reinhardt and physician and global-health expert Adel Mahmoud. He says he became comfortable with ambiguity, as not every potential solution to a policy problem can be tested with the kind of double-blind, placebo-controlled studies that are the gold standard of medicine. And he was inspired by an elective on entrepreneurship with Ed Zschau ’61, a senior research specialist at the Keller Center for Innovation in Engineering Education. Tim Ferriss ’00, the podcast host and author of books including The 4-Hour Workweek and The 4-Hour Chef, made a guest appearance in that class, inspiring Ku to “go outside my lane” and collaborate with people in other specialties. Ku longed to creatively take on knotty problems such as urban homelessness. A lab devoted to thinking like a designer, in a more open-ended, cross-disciplinary way, seemed like one way to do that.
But he had no model for that. And he had no formal training in design, though he’d always been interested in areas such as architecture and clothing design. As a kid, he was fascinated by the variety of fonts included with the then-new Macintosh computer. As Ku and Lupton explain in their book, there are two key principles of design thinking: a human-centered perspective that “starts with the needs and desires of people, rather than with a business proposition or an artistic idea,” and a creative mindset “favoring open-ended exploration.” Over the past 15 or so years, design thinking — with its focus on observation, imagination, and making prototypes — has been popularized by the firm IDEO, the Stanford d.school, and others who have spread the mindset beyond the design world to areas such as business and education.
Ku reached out to those institutions and other design-thinking veterans to learn more about this way of thinking. The approach “blended scientific discovery, merged with the creative mindset of artists,” he says. He loved it. Design thinking had made its way into health care over the past decade, but Ku specifically wanted to create a space for formally teaching design thinking to med students. Doctors-in-training have had to hew pretty close to perfection to make it through the competitive weeding-out processes of college and med-school admissions, and, “No one is used to failing!” says Ku. But, he wonders, if you don’t get used to low-stakes failures like the kind a kid might get on a sports field — or a med student in a design lab — what will happen when you first fail as a physician? What will you do when you confront a stressful decision for which there is no single correct answer? “So much in medicine is not black and white,” says Ku.
To help students develop some of the skills that Ku felt couldn’t be taught in a traditional classroom, in 2014 he created the Innovation and Design Application (IDeA) program at Jefferson. The program accepts a handful of Princeton sophomores each year, who are accepted early to Jefferson’s Sidney Kimmel Medical College; they forgo the MCAT and some premed prerequisites (they attend a science boot camp before starting med school) and participate in the design track while at Jefferson. “Iteration and learning from failure were not something that I was conditioned to see value in for most of my academic life,” says Nick Safian ’17, a Jefferson med student accepted through the IDeA program. “Working in the lab is incredibly freeing,” he says. “You can go to the design lab for a session and not have to worry about getting something wrong or performing for someone who is evaluating you.”
Ku wanted a medical career to be possible for different types of people, with a wider variety of academic experiences and mindsets. Chitra Parikh ’21, who is in the IDeA program and was an HDL intern in 2019, says the program has let her focus on her Princeton architecture major and her independent work in health-care design while also planning for med school.
Students say Ku is a generous mentor, quick to respond and genuinely interested in their work and progress. The culture of the lab is “very group-based, interactive, and hands-on,” and feels less hierarchical than a traditional academic setting, says medical student Ellen (Roop) Solomon ’17, who was also accepted to Jefferson through IDeA. “Bon is one of those people who invests as much in his students as he invests in the lab and in medicine broadly,” says Parikh.
Ku wants to interest even more people in thinking like a designer. He and Lupton, who is the author of a host of design books, met in 2018, at a panel. They hit it off and decided to mount an unusual collaboration to produce what Lupton calls a “handy, accessible, and useful” book that shows how design can be applied to health care, with examples and contributions from a variety of institutions, companies, organizations, and individuals. Now the authors are working on a second edition, updated with COVID-related examples. As an ER doctor, Ku has a unique, front-line perspective on so many of the problems in health care, says Lupton. “It’s where inequity shows the most, where people’s anxiety shows the most, where people are frustrated,” she says.
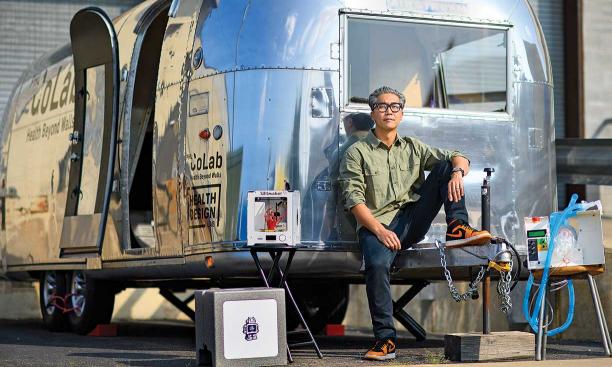
After the HDL was established, Ku wanted to address a question that had dogged him earlier in his career: What can be done to help underserved Philadelphians engage with the health-care system to avoid those regular ER trips? He saw architecture professors at the University of Kansas present their work on community-design projects, including the renovation of an Airstream trailer, and immediately thought that he could do the same thing to bring community health projects to neighborhoods that most needed them. With the help of grants, and with brainstorming by HDL members and Princeton interns, the CoLab Philadelphia program launched in the summer of 2018. Pre-pandemic, Ku hauled the 26-foot trailer behind his Subaru to vulnerable neighborhoods, where, in partnership with community groups, lab members offered services such as health screenings, HIV testing, activities for kids in neglected playgrounds or vacant lots, and a nutrition-education program that includes cooking demonstrations and meal kits. During the pandemic, the Airstream has been used to stage Jefferson’s walk-up COVID-testing program, and this fall it will travel to parking lots in areas of the city with limited access to testing.
COVID didn’t hit Philadelphia nearly as hard as New York City. But it was still terrible and overwhelming. Ku says he worked a Sunday overnight shift and there were no COVID cases. Forty-eight hours later, the ER was full of people showing symptoms, and Ku intubated his first COVID patient. In a New York Times video filmed during the early weeks of the pandemic, Ku calls it “the strangest thing — I never experienced anything like this in my career.” Every patient in the ER, regardless of why they were there, potentially had COVID, and no one had experience identifying or treating the new disease. Frontline health-care workers have been among its victims.
“I respond to stress by doing,” Ku says. The HDL has been a welcome outlet for him and other lab members who felt frustrated and wanted to help, but didn’t know how. Despite the pandemic and racial and socioeconomic disparities in COVID outcomes, he remains optimistic that our health-care system can be made better. He’s especially encouraged by the “frank conversations we are having about racism,” since it drives many social determinants of wellness, including housing, access to transportation, and access to health care. Whether it’s towing the Airstream around the city, thinking about how ERs will need to be redesigned in the age of COVID, or treating patients, Ku considers his best work to be hands-on, and he wants to keep it that way. “I don’t want to be the chef-owner who doesn’t cook on the line,” he says. “I want to cook on the line.”
Katherine Hobson ’94 is a freelance journalist focusing on health and science.


