Sometime on Thursday, Sept. 5, 1918, a young man enrolled in the Navy paymaster’s school on Princeton’s campus reported sick with an upper respiratory infection. At the height of World War I, much of the campus had been transformed into a military camp; the paymaster’s school, which trained clerical officers, was housed at the Graduate College. We do not know the young man’s name — he simply is mentioned in a report — but he was diagnosed with influenza and placed in isolation.
Although the University took pains to isolate anyone suspected of having influenza, the disease spread. By mid-October, beds were lined up in the corridors of McCosh Infirmary, and President John Grier Hibben 1882 made the field house available to isolate some 200 of the most serious cases. Off campus, the situation was even worse. The Princeton Packet reported that more than 300 cases of influenza and 50 cases of pneumonia had been diagnosed in town, and 15 people had died. Before it subsided, the flu would kill 32 Princeton residents. Yet on the campus, it killed no one.
The influenza pandemic of 1918–1920 was the deadliest in recorded history. Striking in three waves during those 26 months, the disease would appear, recede, and then return. It is estimated that influenza killed 5 percent of the world’s population during that period, including 675,000 Americans. The most virulent outbreak was the second wave, which ran from September until early December 1918. Historian John Barry estimates that more than 16 million people may have died worldwide during that lethal autumn 90 years ago.
Princeton was exceptionally fortunate. Fifty-nine University of Michigan students, in contrast, died of the flu that fall. At Dartmouth, one faculty member, five students, and 10 soldiers stationed on campus died. Two died at Harvard, although it had instituted a partial quarantine.
Why Princeton was spared any deaths remains a point of study, as the answers could have important implications in the event of another virulent influenza outbreak or a bio-terrorism attack. The University used a strategy known as protective sequestration, which is designed to protect healthy people from contracting an infectious disease that exists elsewhere. (A quarantine, by contrast, usually is employed to segregate people who are sick, to prevent them from spreading the disease.) In 2005, the Defense Threat Reduction Agency commissioned the University of Michigan Center for the History of Medicine to undertake a study of Princeton and a handful of other places that largely escaped the ravages of the 1918 flu pandemic, to see whether “non-pharmaceutical interventions” such as isolation and protective sequestration are effective. The findings have been reviewed by the Centers for Disease Control, the Department of Health and Human Services, and the Department of Homeland Security. The broad conclusion is that aggressive sequestration seems to be effective in saving lives. But, epidemiologists warn, it’s impossible to discount the possibility that in 1918, Princeton simply got lucky.
Princeton in the fall of 1918 was almost unrecognizable as an institution of higher education, as almost all the old college routines had changed. The eating clubs had closed for the duration of the war, The Daily Princetonian had suspended publication, and the football team played only an informal schedule. Hibben, who had been an early advocate of military preparedness, “lost no time in placing the University’s resources at the disposal of the government” (in the words of Alexander Leitch ’24, author of A Princeton Companion) once the United States declared war on Germany in April 1917, and the faculty unanimously endorsed compulsory military service. Those students who did not enlist immediately joined ROTC, drilled, and studied tactics.
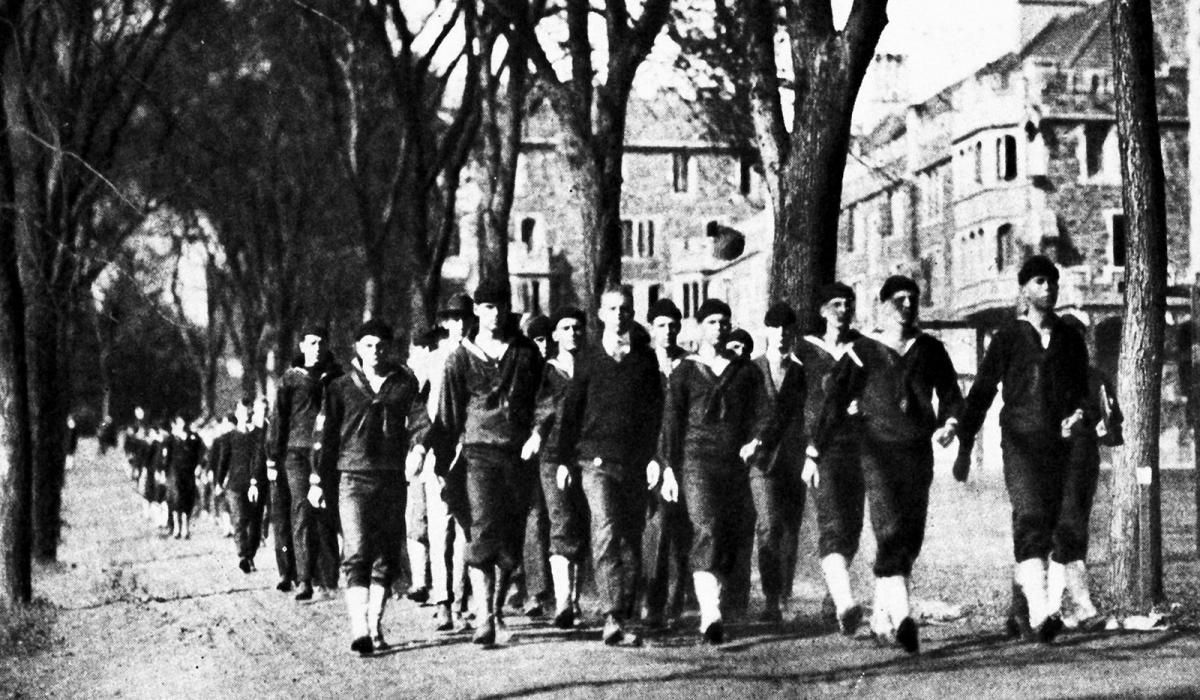
In August 1918, Congress created the Student Army Training Corps (SATC), paying some colleges and universities to host military training camps. By the time classes started at Princeton the next month, 711 students had enrolled in its SATC program under the command of Col. John A. Pearson, a West Point graduate who had been appointed the previous year to teach military science. Another 322 men were enrolled in a naval unit under the command of Adm. Caspar Goodrich, who had won a measure of fame for destroying the enemy fleet at Manzanillo, Cuba, during the Spanish-American War. Six hundred more young men studied in a School of Military Aeronautics. The campus that fall had only 95 regular students, known derisively as the “Diplomatic Corps,” most of whom were either too young to enlist or had some physical impairment.
The first outbreak of influenza occurred at Fort Riley, Kansas, in March 1918. A virus, influenza spreads through human contact; within three weeks, more than 1,100 troops at the fort had become sick, and 38 had died. Military camps were ideal places to spread the virus because men were forced into close contact with each other and then were shipped off to other places, carrying the infection with them. College campuses shared many of the same characteristics.
The flu in 1918 was much worse than a bad cold. Those who caught it could die quickly and often after gruesome suffering. Mucous membranes became so badly inflamed that some patients died when the lining of their stomachs or intestines hemorrhaged. Others bled from their ears or eye sockets. Sometimes the disease inflamed blood vessels in the brain, producing symptoms that resembled a stroke. Indeed, John Barry suggests in his history of the pandemic, The Great Influenza (2004), that a minor stroke President Woodrow Wilson 1879 is believed to have suffered in Paris during the 1919 peace-treaty negotiations actually may have been an attack of influenza.
The usual way influenza killed was, in effect, to drown its victims. As fluid filled a person’s lungs, it displaced oxygen and he or she began to turn blue or even purple, a condition known as cyanosis. A doctor at one military camp described it chillingly. “The men,” he wrote, “start with what appears to be an ordinary attack of LaGrippe or Influenza, and when brought to the Hosp. they very rapidly develop the most vicious type of Pneumonia that has ever been seen. Two hours after admission they have the Mahogany spots over the cheekbones, and a few hours later you can begin to see Cyanosis extending from their ears and spreading all over the face, until it is hard to distinguish the colored men from the white. ... It is only a few hours then until death comes.”
We tend to think of the flu and or other infectious diseases as preying on the old, the sick, and the weak — anyone whose immune system is compromised. One of the most mystifying characteristics of the 1918 pandemic was that it attacked the young and otherwise healthy at a much greater rate. Scientists speculate that this may have been because older people had developed resistance to the virus during an earlier and much milder flu epidemic. Recent research, Barry says, suggests that this strain of the virus stimulated the production of so many antibodies in young people, whose immune systems are strongest, that this very reaction filled the lungs with fluid and choked its victims to death.
By August 1918, when the second wave of the pandemic began, influenza cases were reported simultaneously among troops in France, in western Africa, and at Camp Devens, outside of Boston. Military officials on campus, by now familiar with the disease and its effects on training camps, acted quickly to prevent its spread to Princeton. Adm. Goodrich took the lead, ordering that a disinfecting plant be established at the edge of campus and made available to other military and civilian groups. Each of the 200 men who arrived at the paymaster’s school Oct. 1 from the naval training camp at Pelham Bay Park in the Bronx, where an outbreak had been noted, was ordered to strip. Their outer clothing was placed in a disinfecting room overnight, to be sterilized by exposure to barium dioxide-formaldehyde. The men then had a solution of chlorazene and menthol sprayed into their noses and throats before being given hot baths. Anyone who showed the slightest symptom of infection was dispatched to isolation.
At the height of the epidemic, Goodrich explained his routine in a letter to a colleague in Washington. “I make a practice of inspecting the Battalions every day,” he wrote, “in person or through the Surgeon, to pick out men who appear in the least droopy and send them to the Infirmary for closer examination. It was difficult at first to impress upon the minds of these young men the fact that any cold, however slight, might develop into a serious case. Now, however, they understand and are very prompt in reporting even such a trivial matter as sniffles.”
Though Princeton had isolated the first cases, by early October it was clear that “the epidemic was at hand,” as one report put it. It was at this time that the infirmary beds began to overflow and an emergency hospital at the field house was opened.
Techniques to control the disease were simple. In an order dated Oct. 10, Col. Pearson directed that rooms in Pyne Hall “be thoroughly cleansed with a carbolic acid solution ... The bedding to be hung in the open air for 24 hours, the doors closed and the windows opened for 24 hours.” Goodrich described how doctors treated patients admitted to the emergency field-house hospital. “Walking cases spent their day in the open air under bright sun; cot cases were placed also on the outside to benefit by nature’s therapeutics ... ” The admiral also supervised the creation of a committee composed of representatives from the military training units; Dr. J.M. Carnochan 1896, the chief physician at McCosh Infirmary; and the town health officer. Thanks to their influence, after two local residents had died, the Princeton board of health closed all movie theaters, bowling alleys, and billiard halls, and recommended that the schools be closed as well. Restaurants were required to limit the number of people they served, to avoid creating crowds. Goodrich and Pearson canceled all furloughs to New York, Philadelphia, and Boston, which were experiencing severe outbreaks.
On campus, at least, the strategy seemed to work; by the middle of October, the number of new cases had slowed considerably. But if the outbreak was subsiding on campus, it was not doing so on the other side of FitzRandolph Gate. New orders were issued to prevent everyone from venturing off campus where they might be exposed to the virus. On Oct. 16, Goodrich forbade those under his command to visit any restaurants in town, on pain of court martial. Two days later, guards were posted around all dormitories between 7:30 and 10:30 p.m. and no one was allowed to pass without authorization. In an order dated Oct. 28, Goodrich prohibited all naval men from going anywhere in town east of Bayard Lane or north of Nassau Street without special permission. A subsequent order directed that “men who have passes to go on Nassau Street shall stay on the south side of the street until opposite the place they are permitted to visit. Upon leaving they will return to the Campus at once, crossing the street at right angles.” (It appears, however, that the ban on going into town was often evaded. In one story, a green freshman from the SATC program assigned to patrol Nassau Street discovered two upperclassmen who had sneaked off to Renwick’s ice cream parlor. When he confronted them and demanded their names, they gave him the names of a proctor and the dean of students, which he promptly reported to the corporal of the guard.)
“The campus,” an article in PAW observed, “has changed from a free and easy place within which the night owl might roam, into a well-policed camp.”
Many campus activities went on more or less as normal. When he was not supervising the disinfecting of incoming sailors, Goodrich tried to build their powers of observation by sending them on long hikes through the countryside and then quizzing them in minute detail on what they had seen. Students in his classes had to be able to send and receive up to 60 letters per minute in semaphore, while anyone who forgot to bring a notebook was assigned to write a personal note of apology and to summarize Hibben’s sermon at chapel the previous Sunday. Goodrich’s papers in Seeley Mudd Library contain folder after folder of these punishment letters, all written while the great influenza epidemic raged.
And if students and soldiers were not allowed to leave campus, their parents managed to see them. “As for your visit,” wrote E. Lansing Bennett ’22 to his father Oct. 27, “really, Dad, I can’t say much until the influ is over. Some of the parents came here today, but I don’t think the officers like it much.” Many of the parents came to watch a freshman parade in which John Marshall Harlan ’20 — who would go on to serve on the U.S. Supreme Court but was then the student commander of Goodrich’s naval unit — led a group around campus singing Princeton fight songs. In line behind him was Adlai Stevenson ’22, who wrote later that afternoon to his mother back home in Bloomington, Ill., “I feel sure that the ‘flu’ is not half as bad here as there.”
He probably was right. Influenza, which had arrived in Princeton with such terrifying suddenness, seemed to dissipate almost as quickly. A week after Stevenson wrote his letter, the epidemic had eased sufficiently that Princeton reopened the stores and theaters. Four days later, on Nov. 7, the campus military units lifted all travel restrictions. And four days after that, on Nov. 11, the Armistice was declared. The war was over, and there would be no more need for training camps or protective sequestration. Everyone seemed to want to relax a little, and that weekend, Goodrich led the SATC and naval units in a parade up New York’s Fifth Avenue. The SATC was demobilized just before Christmas and the naval unit placed on inactive duty. When the second semester began on Jan. 6, 1919, Princeton had returned to its regular academic routine.
Although the influenza pandemic continued for another year, it never regained the same lethal potency. There have been subsequent influenza pandemics in the decades since then, in 1957–58 and 1968–69, but neither was nearly as deadly as the one that began in 1918. Even today, though, influenza and pneumonia are the seventh-leading cause of death, killing more than 37,000 Americans a year, and a lethal mutation of the virus like the one that occurred in 1918 remains a possibility. The threat of bioterrorism also makes it particularly important to study whatever steps might be effective in the event of another pandemic.
Peter Johnsen, university physician at Princeton, says he has looked at the University’s experience during World War I as a member of an emergency-preparedness task force, but won’t discuss the task force’s plans in detail. “I can say that Nassau Hall has instructed us to develop planning around this issue, that the [task force] has taken up the issue, and that resources have been allocated,” he writes in an e-mail. (General information about how Princeton would deal with flu and other health emergencies is posted on the University’s web site, at http://web.princeton.edu/sites/emergency/pandemic.htm#plans.)
Howard Markel, the director of the University of Michigan’s Center for the History of Medicine and its study, believes that Princeton’s strategy in 1918 was effective. “It looks like, for a short-term measure, where you don’t have vaccines or antiviral drugs, that this can buy you some time. The question is, can you get people to do it?” A CDC study of the 1918 pandemic, issued in December 2006, concluded, “Princeton University provided a good example of how a social institution with some measure of control over its population might implement NPIs [non-pharmaceutical interventions] to protect itself.”
Princeton, however, benefited in 1918 from several conditions that might not repeat themselves in the event of another outbreak. The military presence on campus made it easier to enforce sequestration, the student body was much smaller, and the town was more isolated from the outside world. Even Goodrich recognized this, writing afterward that “what was done here could not have been done in a large community — especially a manufacturing or commercial community like Boston or New Haven.”
Cleto DiGiovanni of the Defense Department’s Defense Threat Reduction Agency, one of the authors of the CDC’s 2006 study, suggests that we not discount the possibility that Princeton’s low mortality rate was the product of simple luck. “We see this all the time” in epidemiology, he says. “We don’t know why, in a pandemic, some communities are hit hard and other, similar ones are [hit] less so. There are variations in that virus and we don’t know what causes them.”
However, DiGiovanni quickly adds, our uncertainty is not an excuse to do nothing. “It would be dangerously wrong to try to minimize the importance of social-distancing measures as a public-health tool to keep people healthy. The influenza virus travels through the air. If you can minimize the number of people crowded together, some of that virus may fall to the ground rather than falling onto a number of people who will get sick.”
Mark F. Bernstein ’83 is PAW’s senior writer.