It was October 2004, and only his second time on call at his new job in Wisconsin, when Rodney Willoughby Jr. ’77 heard about the patient who would change his career.
A pediatric infectious-disease specialist at Children’s Hospital of Wisconsin in Milwaukee, Willoughby was accustomed to treating young patients with dangerous bacterial and viral invaders attacking their blood, bones, and brains. But he never had treated someone with rabies, and that’s what the physician on the phone said might be afflicting the gravely ill 15-year-old girl who was about to be transferred to Willoughby’s care.
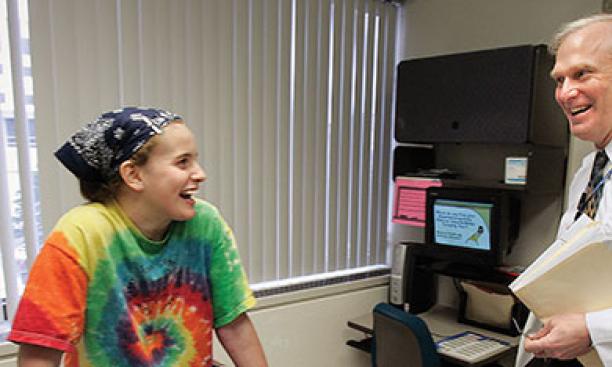
Willoughby had no idea during the subsequent weeks and months of caring for Jeanna Giese that a scientific controversy would erupt over his experimental treatment for her. Giese lived, becoming the first documented person to survive rabies without being immunized. Nonetheless, Willoughby’s novel theory about how rabies kills and the treatment plan he came up with have been hotly contested, and almost a decade later, the debate is far from settled.
Giese lived in Fond de Lac, about 60 miles from Milwaukee. On Sept. 12, she’d gone to Mass with her mother. A bat flew into the church, interrupting the service, and after an usher knocked it to the floor, Giese walked to the back of the church with the intention of releasing it. When she picked it up by the wings, it sank a fang into her finger, where it hung until she pulled it off. At home, she cleaned the wound with peroxide, and the high school sophomore went on with her busy life, which included volleyball games and taking the PSAT. On the day she took the test, in mid-October, Giese fell ill.
First she was extremely tired — too tired to play in a key volleyball game, missing homecoming — and that progressed to double vision, vomiting, excess saliva, and a numb hand. When her pediatrician asked about her medical history, he found out about the bat bite. Speaking to the doctor on the phone, Willoughby recommended the transport team wear protective gear, just in case, though there are no documented cases of human-to-human transmission of the virus — and it wasn’t clear Giese had rabies at all. Giese arrived at Children’s Hospital.
“I’d never seen a case of rabies,” says Willoughby. Few physicians in the United States have. The disease kills about 60,000 people a year, mostly in Asia and Africa, according to the World Health Organization. Only one to three of those deaths are in the United States, because of the widespread vaccination of pets and availability of preventive measures. Most victims in other countries are bitten by unvaccinated dogs, but any mammal can get and transmit the disease, including foxes, raccoons, skunks, and bats.
The rabies virus enters the system through the animal’s saliva and can take weeks or months to move from the nearby tissues and attack its target, the nervous system. Death is preventable if the patient quickly gets post-exposure prophylaxis — wound-cleaning and a multiple-injection rabies-vaccine series. More than 15 million people get that preventive treatment every year, including 40,000 in the United States. But if the patient isn’t treated, the virus eventually makes its way into a peripheral nerve and moves toward the spinal cord and brain. There it wreaks havoc — provoking paralysis and loss of sensation — though no one understands quite how.
“We are no further along in the management of this disease than we were 40 years ago,” says Charles Rupprecht, the director of research for the Global Alliance for Rabies Control and a professor at Ross University School of Veterinary Medicine in St. Kitts. In fact, death from rabies is so accepted, Willoughby recalls that all he needed to know about the disease for his board exams was that it could not be treated. Given that Giese had not been vaccinated and was seemingly in the throes of a full-fledged neurological crisis, if the Centers for Disease Control and Prevention lab confirmed the disease from examining samples of her saliva, skin, blood, and spinal fluid, her prospects were dim.
Willoughby knew that if Giese did have rabies, the normal course of events would be to keep her comfortable until she died. But as his patient lay in the intensive-care unit, he searched for possible treatments. He found little in medical literature about how to treat rabies, because no one had survived. He called a CDC rabies expert to see if any new research findings or treatments were in the pipeline — nothing. From looking at case reports on how rabies killed people, he did find some interesting information: that the brains of rabies victims don’t appear ravaged after their deaths, and that if victims receive life-prolonging assistance to breathe and maintain blood pressure before death, their bodies after death are virus-free.
As Willoughby later wrote in an article in Scientific American, “the rabies virus seems to induce the brain to sabotage the vital organs,” perhaps by overexciting the central nervous system. “I thought, ‘Maybe there is a way here: sedating the patient and buying time” to let the patient’s own immune system work, says Willoughby. “It seems so obvious that you doubt yourself.”
Willoughby read more that night. The next day, Giese was worse. After Willoughby received a rabies confirmation from the CDC, he gathered a group of experts in neurology, critical care, and infectious disease, and proposed a plan: What if they used a cocktail of drugs to sedate Giese during that crucial period? They settled on the sedatives ketamine and midazolam and the antiviral and neuroprotectant amantadine. Rupprecht, then at the CDC, suggested they add the antiviral drug ribavirin as well. (They later added phenobarbital, in small doses, to induce a coma, though that wasn’t part of the original plan.)
Willoughby gave his colleagues a chance to veto his idea, but “no one had a really good reason not to do it,” he says. With his colleagues on board, Willoughby went to Giese’s parents and offered three options: hospice care at home, conventional medical care in the hospital, and what Willoughby calls “this improvised therapy,” which was “an idea but had zero data” behind it.
Willoughby knew that his third option was a risky proposition. The drugs had toxic side effects. Even if they worked, Giese might survive with severe neurological impairment. Her parents, he remembers, were “remarkable.” They opted for the experiment, saying that perhaps science — and future patients — would benefit, even if Giese didn’t survive. Despite his plan of attack, “I had the expectation that she would die,” says Willoughby.
While Giese was in an induced coma, the waiting was unbearable, recalls Willoughby. After about a week, it was time to taper off the sedation and return her to consciousness. “Those were the scariest days of my life,” Willoughby says. At first she was fully paralyzed, but she had electrical activity in the brain and pupils that reacted to stimulation. “I thought I’d done the worst thing and created someone who was locked in,” or conscious but almost totally paralyzed, says Willoughby. “I am pretty sure I cried.”
But over the days, as doctors withdrew the anesthesia, Giese’s reflexes slowly returned. Within two weeks she was sitting up and looking around, and she began a long, difficult recovery filled with rehabilitation to relearn, as she says on her personal website, “how to speak, walk, stand, pick things up, point, eat, drink, everything a baby learns.” She left the hospital in January 2005. A year after her diagnosis, she gave a speech at an international gathering of rabies researchers, and in 2011 she graduated from college, with Willoughby in attendance.
Still, because nothing was known about rabies recovery, and it was possible that Giese would relapse or suffer long-term complications, Willoughby says he didn’t breathe a sigh of relief until about two years after her treatment. “We didn’t know if there was a second train coming down the tracks,” he says.

And in the meantime, he had plenty of questions. Why did Giese survive? Had she been infected by a mild or unusual form of the bat-rabies virus? Or did the protocol save her? And if so, which elements were responsible? Would the approach work for other rabies victims?
Willoughby and his colleagues reported Giese’s case in the CDC’s Morbidity and Mortality Weekly Report and, in 2005, in the New England Journal of Medicine. The Medical College of Wisconsin set up a website with the detailed treatment regimen — which became known as the Milwaukee protocol — as well as a registry where clinicians could record the details of their experience using the protocol. Willoughby expected that with tens of thousands of fatal cases of rabies a year, other physicians would start using it and “we’d have an answer within six months.”
That didn’t happen. “I’m puzzled by it, frankly,” says Willoughby. Many rabies researchers rejected the notion that the protocol is what saved Giese, saying the treatment was unethical and wouldn’t lead to any more survivors. And indeed, when it was tried in the first few years after Giese’s case, patients died. (Willoughby says the protocol wasn’t followed strictly in about half of the cases.) There have now been 51 known attempts, with seven survivors including Giese. Of them, five are still alive, though one is severely impaired and two have some impairments, says Willoughby.
Clearly the protocol doesn’t work for everyone. Its critics argue it doesn’t work for anyone, and harms patients who already are suffering greatly from the terrible symptoms of rabies. “‘Do no harm’ is the ancient dictum that physicians are expected to abide by,” says Henry Wilde, a doctor on the faculty of medicine at Chulalongkorn University in Bangkok, who unsuccessfully tried the protocol with his colleagues on a dog-bite victim. “What was largely done in the original Willoughby protocol may well have done some harm, yet that girl still recovered due to her vigorous defenses against the virus” and excellent intensive life support, he says, adding that all the patients who have survived showed evidence of a “very great natural-defense mechanism.” What Willoughby’s work highlighted, Wilde says, is that “rabies is not invariably fatal,” adding that survivors likely have gone undiagnosed over the years.
That is the heart of recent arguments against the Milwaukee protocol: The handful of survivors would have lived without it. There is evidence to support the idea that infection isn’t always fatal. Not all afflicted animals die from the disease, and research in remote areas of Peru where infected vampire bats are common has found that some people have antibodies against rabies despite never having been vaccinated — suggesting previous, non-fatal exposure. (Willoughby says that is most likely to happen in small indigenous populations where rabies is endemic.) And there is the case of the Texas “wild child,” a 17-year-old girl, believed to be a runaway, who was admitted to a hospital in 2009 with symptoms consistent with rabies and reported contact with bats. Certain aspects of her case and lab tests indicated rabies; she got one dose of the vaccine but no more, because of concerns that it would only exacerbate her illness. She never required intensive care and left the hospital, returning a few times because of headaches. But she didn’t return for more follow-up care, and public-health authorities don’t know where she is or how she’s faring.
Willoughby points to the numbers to argue that his approach merits further study. While a 14 percent survival rate is low, it’s better than the one possible survivor noted among 77 case reports describing other attempted treatments (using other methods, including ICU care) he’s seen reported in listservs and in medical literature. Willoughby says these reports aren’t perfect, but they are the closest to a control group that he has.
Willoughby says he is open to the possibility that certain elements of the protocol cause harm. He and his colleagues already have tweaked it several times, and he hopes to refine it further to improve efficiency and safety. It also might be possible to develop a stripped-down version for less severe cases in areas lacking ICU care. “A lot of people are almost surviving but for the fact that they didn’t have an anesthesiologist” to sedate them and give the body more time to respond, he says. He also would like to conduct human trials comparing the protocol to more standard intensive care. (While animal studies would be ideal, he says, it’s not possible to simulate intensive care for mice, and veterinary schools were not receptive to the idea of treating rabid animals such as dogs, he says.)
Critics don’t think the protocol is worth studying or using at all. “Use of this protocol should ... be discontinued,” says the University of Manitoba’s Alan Jackson in a 2013 review published in the journal Antiviral Research. Wilde says his local rabies consortium has opted to provide standard ICU care, including ventilation and blood-pressure support, to as many patients as possible who show an immune response, as measured by rabies antibody in the spinal fluid and a lack of rabies RNA in any body fluid. None have survived.
The conference at which Giese spoke on the anniversary of her diagnosis, the annual Rabies in the Americas meeting, has become a key place to hash this out in person. Willoughby expected more debate when he traveled to Toronto in October for the 2013 conference. Sergio Galvez, a physician from Chile, presented a recent case in which a 25-year-old man was bitten by street dogs and given one dose of the rabies vaccine. Less than two weeks later, the young man showed symptoms of rabies. He survived after being treated in accordance with Willoughby’s protocol and put on a ventilator.
But the latest presentation was met by only a few questions. “It’s calmed down a lot,” says Willoughby, settling into a hotel lobby chair on the first day of the conference. The lack of sparks also might have been due to the fact that Willoughby himself wasn’t presenting the case. He came to the meeting to hear Galvez’s presentation, and also because it’s the one week each year when he can focus solely on rabies. His usual workflow includes his clinical practice, and he also sits on national committees that recommend vaccine policies. Before the Giese case shifted his course, he was doing research on whether cerebral palsy might be related to prenatal infections, but that has fallen by the wayside.
Willoughby seems unfazed by the rabies debate, which he describes as “anecdotal and personal” because of the small rabies-research community and by the limitations of the case reports that track the protocol’s use. He is not used to giving up; if someone tells him he can’t do something, he says, it often just stokes his will.
So the debate continues. The CDC’s online information on rabies advises clinicians that they can “either offer supportive therapy or an aggressive treatment plan. There is no single effective treatment for rabies once clinical signs are evident.” It provides two links: one providing information on Willoughby’s Milwaukee protocol; the other, a 2002 article on case management suggesting that rabies is 100 percent fatal. Rupprecht thinks it’s worth having a major symposium that brings together all the experts to “hash out a protocol and a new way to move forward,” and to figure out “what’s state-of-the-art and what we’re prepared to do.” He says he’s “a firm believer that we can intervene.”
Willoughby and his critics do agree on one key idea: Treatment is not the best solution to the problem of rabies. As it stands now, it’s a last-ditch attempt, and an expensive one at that. The cost of providing care for one case in Bangkok was equivalent to the amount of money needed to give pre-exposure vaccination to 30,000 children in that city, Wilde says. Willoughby estimated the cost of Giese’s care in 2004 at $800,000 or more. Prevention is far more efficient. In addition to consistently providing post-exposure prophylaxis to people bitten by wild animals, “if you could control dog rabies and the dog population, you’d not need this,” says Willoughby.
Researchers at Thomas Jefferson University in Philadelphia are researching a single-dose combination rabies vaccine and contraceptive shot for dogs, with funding from the Bill & Melinda Gates Foundation. The “One Health” approach to rabies and other zoonoses — diseases that spread from animals to humans, including West Nile virus, avian flu, and HIV/AIDS — is based on the notion that animal, human, and environmental health are linked, according to Laura Kahn *02, a physician and research scholar at the Woodrow Wilson School. “You want to control the disease at its source, rather than waiting for the human to get accidentally exposed,” she says. “By targeting the health of animals, you include the health of humans.”
But even if better vaccines are developed, that doesn’t mean research on treatment — including his protocol — should end, says Willoughby. “You always need a plan B,” he says.
Katherine Hobson ’94 is a freelance writer specializing in science and medicine.


