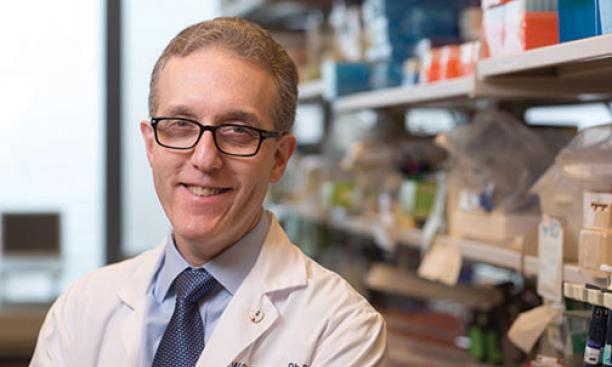
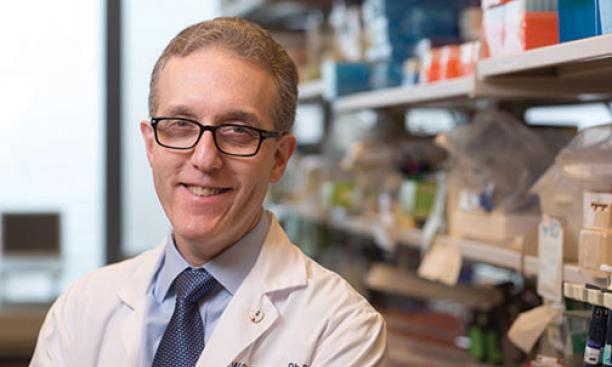
With his boyish appearance, Jedd Wolchok ’87 could be mistaken for a medical resident. But he is an oncologist and an immunologist at Memorial Sloan-Kettering Cancer Center in New York who has spent 25 years studying how drugs and vaccines could arm the immune system to fight cancer.
A leader in the immunotherapy field, he is at the center of the development of a new class of drugs that could provide a turning point in cancer treatment. The currently available immunotherapies work only in a tiny fraction of patients with certain types of cancer and must be given by experienced immunotherapists. But the newer therapies being tested in clinical trials so far have worked on a larger patient population and in more types of cancer, including lung cancer, the second most common cancer in the United States.
This new generation of drugs is poised to introduce immunotherapy to the rest of the cancer world in a major way, according to Keith Flaherty, an oncologist at the Dana-Farber/Harvard Cancer Center in Boston.
White blood cells can recognize and attack a tumor. However, tumors have ways to evade these immune cells, including boosting the activity of certain molecules that can suppress the activity of immune cells. The new class of cancer drugs — antibodies that block this negative activity — can extend the lives of some patients with cancers previously considered to be terminal by years.
Until a few years ago, immunotherapies were marginalized, considered complicated treatments administered at few cancer centers. Success rates were low, and the therapies could be given only to otherwise healthy patients who could tolerate the autoimmune effects of an unleashed immune system. There was little evidence that more than two tumor types could be treated this way.
But for Wolchok, immunotherapy has been a question not of “if” but “when.” “I saw that it wasn’t a question of whether it was real, but a matter of making the clinical successes more frequent,” says Wolchok, a melanoma specialist at Sloan-Kettering’s Ludwig Center for Cancer Immunotherapy.
Wolchok’s start in tumor immunotherapy traces back to the summer after his freshman year at Princeton. He spent that summer at Sloan-Kettering working with Lloyd Old, considered the father of modern tumor immunology. After completing medical school and a residency in New York, Wolchok returned to Sloan-Kettering to study what happens to the immune system during cancer and how to stimulate immune cells to recognize tumors as foreign.
Wolchok took part in clinical trials that showed, in results released in the summer of 2013, that the new, still-experimental drugs, called anti-PD-1 and anti-PD-L1 antibodies, substantially shrank tumors in one-third to one-half of patients. One trial reported that 43 percent of advanced melanoma patients were alive two years after starting treatment. (Typically, only one-fourth to one-third of advanced melanoma patients remain alive for that long.) The newer drugs minimize the toxic autoimmune side effects such as colitis and hepatitis that have been linked to other immune therapies, and can be given in an oncologist’s office rather than in a hospital.
The new drugs appear to work not only in kidney cancer and melanoma, which historically have been more responsive to immunotherapy, but also for the first time in lung cancer, according to recent clinical trial results. They are being tested in other tumor types. Larger trials needed to approve the therapies in the United States and around the world are underway.
Long-lasting therapy needs to work with the immune system, which has a memory, says Wolchok, and can evolve along with the cancer, similar to children’s vaccines that continue to work for decades. “I am extremely pleased that cancer immunology is changing from a speculative science into a conventional therapy,” he says.
