
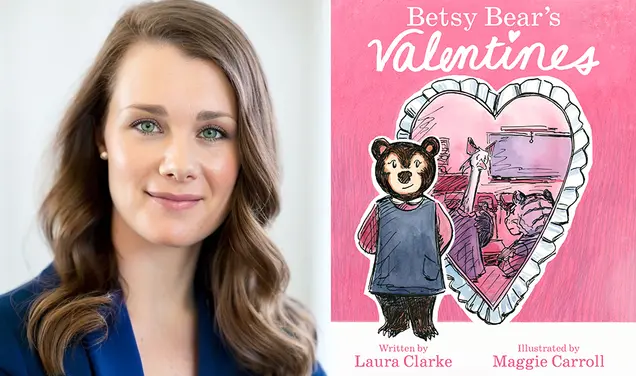
‘A Compassionate Realist’
Dr. Elizabeth Ryan ’00 is on the front lines battling the opioid epidemic
On a typically busy Monday morning, Dr. Elizabeth Ryan ’00 sees a long line of patients at the REACH clinic in downtown Ithaca, N.Y.
Greg, 26, complains of mild chest pain and constipation. Jeffrey needs a tetanus booster and a flu shot but does not want to get them. Amy, who has a thyroid problem, also needs to quit smoking. Joanne, in her mid-40s, is moving out of the state and wants prescriptions filled before she goes. Michael, a weight lifter, reports that he has cut back to smoking only at night. Ryan takes out her stethoscope, listens to his heart, and gives him a high five. (All patients’ names have been changed.)
This is the routine practice of a primary-care physician, which is what Ryan is. But there is an additional layer to the story in each examination room. Greg is on Suboxone, a partial opioid activator, to curb his addiction to fentanyl. So is Jeffrey. Amy was recently paroled from prison, where Nalaxone, an opioid antidote, was impossible to get but heroin was abundant. Joanne was hooked on opioid pills for 12 years before switching to heroin. Now clean, she too takes Suboxone, along with Adderall, Klonopin, and a host of other medications to treat her many illnesses, including hepatitis C.
“I just want to get off all this [medication],” she tells Ryan. “But if I have to take Suboxone for the rest of my life, I will.”
Out in the waiting room of the old frame house that serves as REACH’s home, small cards line the walls, printed by the Drug Policy Alliance. They read: “[X] Should Be Alive Today,” each with a different name written in by a patient or doctor. There are dozens of them.
The opioid epidemic is a war being fought on many fronts: legal, social, political, economic, and medical. Even as its causes and cures are being debated, its effects are undeniable. According to the National Institute on Drug Abuse, more than 130 Americans die every day of an opioid overdose, an annual total greater than the number who die in automobile accidents. Drug overdose, mostly due to opioids, is now the leading cause of death among Americans under the age of 50. The Centers for Disease Control estimates that it costs the country $78.5 billion a year in additional demands for health care, lost productivity, treatment, and law enforcement.
Ryan’s practice is a small part of a large front in that war, but one that she and others insist is critical. Though all of her patients are struggling, Ryan sees their addiction as only part of their medical history. They also require cancer screenings and chest X-rays, flu shots, and tetanus boosters. They need to stop smoking or eat better to keep their diabetes under control. They are people, and not just addicts.
The REACH Project was founded in February 2018 as a nonprofit to provide primary care while also helping patients overcome opioid addiction. The name is an acronym standing for Respectful Equitable Accessible Compassionate Healthcare. Ryan stresses each one of those adjectives.
“The heart of our mission is to bring health equity to persons who previously had not experienced it,” she says. Opioid patients, many of them poor, face numerous barriers to care, ranging from a lack of health insurance to a lack of transportation, but Ryan says that the stigma attached to addiction does just as much to keep them from seeking needed treatment. Someone with hepatitis might need to get blood drawn but resists because she is ashamed of the track marks on her arm. An opioid addict with chest pains might avoid calling 911 because the paramedics treat him as if he is looking for drugs.
Many health-care providers see only the addiction and not the patient behind it, Ryan says. REACH’s goal “is to use the door of the opioid crisis to create an accessible clinic focused on harm reduction, where people could get back into medical care, get the care they deserved, and be treated well.”
Note the words “harm reduction,” not “harm elimination.” Ryan calls herself a “compassionate realist” who recognizes that her patients may not be able to beat addiction completely. “If we’re not going to get perfection,” she says, “I still want to get better than where we are now, and I’m going to work with you collaboratively to figure out the tools that will help you do that.”
As she moves through her morning rounds, Ryan does just that. In each examination, she is friendly but focused, tapping out notes and ordering prescription refills on her laptop. The next patient she sees, a young home-health aide, is suffering from anxiety, post-traumatic stress disorder, and acid reflux on top of her opioid addiction — and wants to tell Ryan about all of it in rambling detail. Ryan listens politely but knows when to step in with a probing question to get the information she needs and steer the visit along.
Respect, though, is not the same as gullibility. Ryan knows that addicts lie about their behavior, but she is convinced that the more she shames them, the more they will conceal — if they come in at all. She neither confronts patients nor takes them at their word, but tries to tease out the truth while assuring them that they won’t be turned away for telling the truth. The goal, she says, is “dealing with patients as people, dealing with problems as problems, and not making assumptions about the person based on the problems.”
Opioids are a class of drugs that affect receptors in the brain regulating pain and emotion. They range from prescription pills such as OxyContin, Vicodin, and Percocet to heroin. All can be lethal, highly addictive, and hard to overcome once someone is hooked.
Epidemiologists trace the opioid epidemic to the 1990s and an aggressive marketing campaign by pharmaceutical companies that urged doctors to treat pain using powerful new opioid-based drugs. Those drug companies, which now face hundreds of millions of dollars in lawsuits, assured the public that drugs such as OxyContin were not addictive, while suppressing evidence that they were. Doctors overprescribed the pills and patients abused them.
A surge in heroin abuse followed, driven in part by people who could no longer obtain prescription opioids. Today, the greatest threat is fentanyl, a synthetic pain reliever administered in a transdermal patch that can be 50 to 100 times more potent than morphine. Much of it is made in China and smuggled into this country.
Few of the patients Ryan sees got hooked on opioids because someone over-prescribed pills for pain relief; most also have problems with methamphetamines, cocaine, or other drugs. “I’ve seen very, very few people who have had emotionally and economically stable lives who accidentally and quickly got addicted to opioids,” she says. The source of the problem runs deeper.
Studies by Princeton professors helped bring the simmering opioid crisis to broader public attention. A 2015 paper in the Proceedings of the National Academy of Science by Anne Case *88 and Angus Deaton reported that mortality rates for middle-aged whites rose steadily between 1999 and 2013, particularly for those without a college education. This coincided with a sharp rise in suicides, cirrhosis of the liver, and opioid abuse, they said. In 2017, Professor Alan Krueger wrote in a paper for the Brookings Institution that nearly two-thirds of all men between the ages of 25 and 54 who were not in the labor force took some form of prescription pain medication every day.
Case and Deaton described the surge of overdoses and suicides as “deaths of despair,” a phrase that has stuck in the public imagination. “Opioids are like guns handed out in a suicide ward,” they wrote in a 2017 op-ed for The Washington Post. “They have certainly made the total epidemic much worse, but they are not the cause of the underlying depression.” They attributed that to government economic and policy choices, specifically those that led to a decades-long stagnation in wages and a loss of manufacturing jobs.
“That gets a solid, ‘Hell yes!’ from me,” Ryan says of this assessment, which fits with what she has seen in her own practice. The problem is especially severe in rural areas like upstate New York. Small communities don’t have addiction-treatment programs or doctors certified to prescribe drugs to treat opioid abuse. They often don’t have the infrastructure to help poor residents hold their lives together, such as well-paying, steady jobs, adequate housing and education, and accessible public transportation.
“It is a sign of our failure as a society to support people with healthy tools for relationships, work, and life,” Ryan says. “I think this is a poverty problem and a mental-health problem. We see lots of rural patients with terrible job prospects and not a lot of compelling alternatives. [Drug use] provides a relief.”
Her commitment to her practice and her patients notwithstanding, Ryan has always been a hard person to pigeonhole.
After focusing on psychology and women’s studies at Princeton, where she captained the rugby team, she returned home to Ithaca and spent the next five years working as an ambulance dispatcher. She spent part of that time living in a local firehouse; after going on calls a few times, she decided to become a volunteer firefighter as well, and later a paramedic.
Being a paramedic, she recalls, “taught me that I didn’t like dropping people at the ER and wondering what happened to them. I wanted to know more.” Changing course again, Ryan decided to become a doctor.
She went to medical school at Boston University intending to practice emergency medicine, but found herself drawn to public health and family medicine instead. “I realized that I loved people’s stories and [getting] the full sense of their lives and families too much to do anything else.” She received a scholarship from the National Health Service Corps for students planning to practice primary-care medicine in underserved areas. While completing her family medicine residency in Seattle, she also learned wilderness medicine and even spent time assisting the Mount Baker ski patrol.
After moving back to Ithaca five years ago, Ryan worked in several private practices. A few opioid patients had come in, but they were not a significant part of her caseload, and she lacked the certification to prescribe opioid-replacement drugs. Still, she was immediately interested when she heard about REACH. After working part time for several months with the clinic’s founder and medical director, Justine Waldman, Ryan joined the staff full time last fall as the associate medical director.
REACH is a clinic, although it can also seem like a social-services agency. Staff members sometimes help patients fill out applications for low-income housing, and a closet in the cramped hallway contains bins of donated clothes for those who need them. Primary-care medicine and opioid-replacement therapy, though, form the bulk of the practice.
Suboxone, the drug Ryan most often prescribes for her patients, contains two other drugs: buprenorphine, which cuts opioid cravings and withdrawal symptoms, and Nalaxone, which reverses the opioid high. A controlled substance, Suboxone is itself an opioid, but it provides less of a high, is less addictive, and is less prone to overdose than other drugs. It usually comes in a dissolvable strip that is placed under the tongue. Patients can take it indefinitely, in effect treating opioid addition as a chronic disease to be managed for life, like diabetes.
In 2013, The New York Times called Suboxone “the blockbuster drug most people have never heard of,” with annual sales exceeding those of Viagra or Adderall, but it also has its downsides and its skeptics.
Addicts sometimes sell their Suboxone prescription on the black market. Though it is harder to overdose on than OxyContin, it is not impossible. Physicians have also overprescribed Suboxone just as they overprescribed opioids.
To combat such abuse, New York state requires that prescribing physicians be certified and limits the number of prescriptions they can write. It also checks to make sure patients are filling their Suboxone prescriptions. Ryan says most of her patients go straight to the pharmacy after leaving her office — “because otherwise they feel like [expletive] and go into withdrawal.” She dismisses criticisms of Suboxone as overblown and says that its limited availability is a greater problem than occasional misuse.
Opioid-replacement drugs have been proven to be effective. In France, overdose deaths fell by 79 percent after buprenorphine became available. The World Health Organization and the National Institute on Drug Abuse endorse its use. But it is hard to get, particularly in upstate New York, which is one reason Ryan’s patients come from 22 surrounding counties. A 2017 report by the President’s Commission on Combating Drug Addiction and the Opioid Crisis found that nearly three-quarters of the rural counties in the United States have no physician licensed to prescribe buprenorphine.
Some critics of opioid-replacement therapy say physicians should get addicts to quit drugs rather than try to manage their use.
“Show me how,” Ryan responds. “It’s not going to be by inducing shame. It’s not going to be by arresting the people who sell it, because people will always make and find it. It’s not going to be by drug testing everybody weekly and shortening leashes in medical care, because I have seen that drive people out of care. [Opioid-replacement therapy] is the most effective way, and it also happens to feel humane and gratifying to me.”
Ann Kurth ’84, dean of the Yale School of Nursing, says the cold-turkey approach misunderstands the nature of addiction. “We should use whatever tools we can to get people to reduce the harm and stop if they are able — but you have to meet people where they are. People need options.”
Ryan thinks of opioid-replacement therapy with another one of her patients in mind. Using Suboxone, “he can focus on his law-school application instead of putting all his energy into resisting heroin.” The drug, she believes, “lets people be normal. And it is as long term as you want it to be.”
REACH is moving across town to a much bigger facility this fall. Two large grants from the state of New York will enable the clinic to expand its mental-health services, hire a part-time psychiatrist and a full-time social worker, and train other area doctors in opioid-replacement therapy.
Recently, Ryan and her staff went through their waiting room and took down many of the cards bearing the names of opioid victims. They replaced them with something more hopeful, a new set of cards that read: “Since Joining REACH, I Have Been Able To: ...”
On each one, the space below is blank, just waiting to be filled in.
This is an updated version of a story in the May 15, 2019, issue. The corrections clarify details of Ryan’s professional background and the description of Suboxone.
Mark F. Bernstein ’83 is PAW’s senior writer.





3 Responses
Robert J. Saner II ’69
6 Years AgoFighting Addiction
Congratulations to both author Mark Bernstein ’83 and subject Elizabeth Ryan ’00 on a very balanced look at the opioid challenges facing the country (cover story, May 15). Unlike many media outlets’ efforts to simplify by focusing almost exclusively on “bad doctors” and “bad drug companies,” your piece gets at the deeper societal issues that underlie this “epidemic,” just as they have underlain previous experiences with different drugs. And it nicely debunks the notion that pills legitimately prescribed for pain, and taken as directed, lead straight to fentanyl-induced overdose deaths on the street. Keep up the good journalism, author; and keep up the compassionate care, subject!
Jerome P. Coleman ’70
6 Years AgoFighting Addiction
Dr. Elizabeth Ryan is indeed a compassionate realist. Her record of selfless educational advancement in the quest to professionally assist others is inspirational. She is the apogee of service to humanity. I would expect no less from a former Princeton rugby captain.
Patrick Doyle
6 Years AgoAn Uplifting, Solution-Based Story
“It is a sign of our failure as a society to support people with healthy tools for relationships, work, and life,” Ryan says. “I think this is a poverty problem and a mental-health problem. We see lots of rural patients with terrible job prospects and not a lot of compelling alternatives. [Drug use] provides a relief.”
So true, yet misunderstood by so many. Our drug-control policies result in only harm, as they do nothing to address this; hence they are failing, and loved ones continue to suffer and die.
To find real solutions, it is important to amend the following statement by adding that pharma is not alone. The Joint Commission on Healthcare Organizations' campaign "pain the fifth vital sign," Medicare/Medicaid tying claims reimbursement to patient reports of pain relief, and our continued failure to adequately regulate pharma marketing and business practices all put heavy pressure on MDs to Rx opioids.
Epidemiologists trace the opioid epidemic to the 1990s and an aggressive marketing campaign by pharmaceutical companies that urged doctors to treat pain using powerful new opioid-based drugs. Those drug companies, which now face hundreds of millions of dollars in lawsuits, assured the public that drugs such as OxyContin were not addictive, while suppressing evidence that they were. Doctors overprescribed the pills and patients abused them.
Excellent piece. Dr Ryan is a credit to Princeton.