
Hearts and Minds
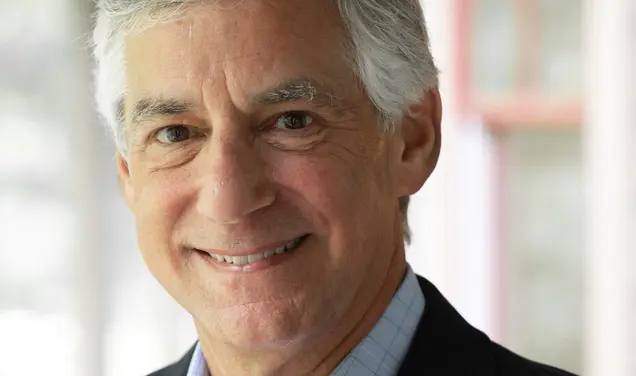
Directing a landmark study of heart disease, Herman Taylor Jr. ’76 took on more than medicine
Watching Herman Taylor Jr. ’76 during the 15 years he spent in Mississippi, it would have been reasonable to conclude that he was running for office. He has ridden in the back of a pickup truck during a parade, given radio interviews, and participated with community leaders in a three-point halftime shootout at a college basketball game. Strangers scrutinize his menu selections. At a lunch on the campus of Jackson State University in May, Taylor is a magnet, repeatedly interrupted by people hoping to catch up on his news.
While he is something of a local celebrity, Taylor is no political candidate — he’s a cardiologist. Since 1998, he headed the Jackson Heart Study (JHS), the most ambitious investigation ever to be done into heart disease among African-Americans, and a project entwined deeply with the community.
The pickup truck, radio interviews, and basketball game? All were tools for recruiting patients to participate in the heart study. As for lunch, Taylor chooses salad, redfish with shrimp sauce, and a Coke. “Oh, people watch what you pick,” he says.
That lunch was among the last that Taylor was to have in Jackson, as he moved in July to the Morehouse School of Medicine in Atlanta. There, as the heart study continues in Mississippi, Taylor hopes to build on the study’s findings — a mountain of data that he characterizes as “a treasure trove of unusual depth and breadth.”
Those data, which Taylor says have only begun to be analyzed, already have helped to provide insights into the disproportionate burden from heart and vascular disease borne by African-Americans. While the overall U.S. death rate from heart disease has declined since the late 1960s because of better prevention, diagnosis, and treatment, “there are still pockets of communities that haven’t enjoyed the fruits of all that biomedical research,” says Gary Gibbons ’78, director of the National Heart, Lung, and Blood Institute, which is part of the National Institutes of Health and funds the heart study.
African-Americans get heart disease earlier and have worse outcomes. In 2010, blacks were 30 percent more likely to die from heart disease than non-Hispanic whites, according to the U.S. Centers for Disease Control and Prevention. Some of the reasons for the disparities are known, but many are not. The JHS was created to ferret out those crucial factors, from genetic variations that are more common among African-Americans to lifestyle habits like diet and exercise to racial discrimination and socioeconomic factors that may affect health. Moreover, taking a hard look at a high-risk population could lead to answers to nagging questions about heart disease that are broadly applicable.
Taylor was drawn to Jackson by a 1998 phone call from Dan Jones, a physician at the University of Mississippi Medical Center (UMMC) and the principal investigator of the nascent study (and now the chancellor of the University of Mississippi), asking if he’d be interested in heading up the JHS. Taylor, who was working at the University of Alabama in his hometown of Birmingham, was initially reluctant. “I had a great job, I was home, I had a great situation,” he says. But Jones was persuasive about the potential of the study to help understand the racial disparities in heart disease. A working group convened by the NHLBI noted in a 1995 report that attempts to explain the difference between coronary heart-disease prevalence and outcomes in blacks and whites were hampered by “the scarcity of comprehensive data” on the disease among blacks. And now the NIH was willing to fund a major effort to gather that data — a multi-year tracking of a sampling of Mississippi’s African-American residents that would gather information on a variety of risk factors and would follow their health status over many years.
The medical center and two of Mississippi’s historically black educational institutions, Jackson State University and Tougaloo College, a private liberal-arts college, would come together to work on the study and also to engage black high school and college students in public health and epidemiology by exposing them to fields in science and technology and research opportunities. That would serve twin goals of “advancing the science as well as the diversity of the scientific workforce,” says Gibbons.
The paragon of this kind of long-term, epidemiological research is the Framingham Heart Study, which started in 1948 with 5,209 participants and since has expanded to include their children and grandchildren. When the study began, Framingham, a small town outside Boston, was populated mostly by people of Italian, Irish, and English descent, with very few African-Americans. (The study started recruiting more ethnically diverse participants in 1994, reflecting the demographic changes in the community.) That study yielded crucial findings about the risk factors for cardiovascular disease — such as research showing that high levels of HDL cholesterol, now known as “good” cholesterol, are beneficial — but no one had taken a similarly in-depth look at the demographic group — African-Americans — that suffered so disproportionately from heart problems.
Mississippi, which has the highest percentage of African-Americans of any state, at 37 percent, was a natural laboratory for such a study. It ranks second-worst in the United States for three key risk factors for heart disease: obesity, diabetes, and high blood pressure. In 2012, almost 35 percent of adults in Mississippi were obese (behind Louisiana), and 12.5 percent had Type 2 diabetes (behind West Virginia). According to 2011 data, 39 percent had high blood pressure (behind Alabama). There are some glimmers of hope in recent data on child obesity in the state, Taylor says. Still, culturally, the South lags in healthful lifestyle measures: “We can take broccoli and turn it into a cardiovascular risk factor,” says Taylor ruefully.
Jackson, the state capital, brought unique advantages to the study. It already was one of the sites in another epidemiological study looking at the risk of atherosclerosis, or hardening of the arteries, and those participants would provide a starting point for the new research. In addition, says Taylor, the three counties involved in the study — Hinds, Rankin, and Madison — are socioeconomically diverse, and the study would attempt to get a representative sample of the Jackson metro area’s African-American population. (In that goal, the study got very close, says Taylor.) That would help disentangle the impact of race in participants’ health from the impact of income, education level, and access to health care.
Taylor knew he would have to mount a major community-outreach effort to recruit and retain participants. Scientific studies requiring time-consuming exams and intrusive questions generally are tough to recruit for. But there’s an additional layer of skepticism among many in the African-American community about government-sponsored medical research. One major reason for that suspicion: the 40-year Tuskegee syphilis experiment, which observed but did not treat the disease in black men — even after penicillin was a known cure. (Then-President Bill Clinton formally apologized for the experiment, which began in 1932, on behalf of the United States in 1997.)
A 1990 survey administered to more than 1,000 African-American churchgoers by the Southern Christian Leadership Conference found that 35 percent of respondents believed AIDS was a form of genocide against blacks. And community surveys in Jackson, done ahead of the recruiting effort, found that residents there had questions, too. “There was some hesitancy about why and what researchers are looking for, and what they are going to do with the information and specimens,” says Donna Antoine-LaVigne, principal investigator of the JHS Community Outreach Center.
So study organizers knew they’d have to explain the benefits of their research to prospective participants, and also to involve them in important decisions in a very real, not cosmetic, way. Recruiters and interviewers were drawn from the African-American community — they were not outsiders. Recruiters reached out to community leaders, to ministers, to barbershops, and to professional medical organizations to draw participants from places like metro Jackson and rural Sharon, population 1,406. Taylor was pictured in The Clarion-Ledger, Jackson’s local paper, alongside the city’s first African-American mayor as the mayor underwent an echocardiogram. Antoine-LaVigne remembers how Taylor showed up when study organizers held holiday celebrations for participants, attempting to maintain their participation.
Before the study began, there was an effort to inform the community about the health disparities it was trying to decipher. One print ad, featuring an older African-American couple, says, “Don’t Let the Photo Album Be the Only Thing You Leave Your Children.” It continues: “African-Americans have higher rates of high blood pressure, heart disease, stroke, and kidney failure than the rest of the population. In Mississippi, more than a third of all African-American deaths are from cardiovascular disease. The Jackson Heart Study wants to change that so you can leave a legacy of good health for future generations.”
“Before we did the science, we let people know the study was about them,” says Taylor. And people got it. “They said, ‘This may not help me, but maybe it will help my children.’”
For Taylor, heart and circulation problems have struck close to home. He grew up in Birmingham, where his father, a steelworker, developed high blood pressure at the age of 29. (The salt tablets his father consumed to replace lost sweat probably didn’t cause the hypertension, but they didn’t help either, says Taylor.) Both of his grandmothers had strokes. That family history was one of the factors that drew him to cardiology as a specialty after studying biology at Princeton and medicine at Harvard. A summer fellowship at Cornell Medical School in New York between his junior and senior years of college, where he was exposed to the physiology of cardiology, strengthened Taylor’s interest. “It just made sense to me,” he says.
Ultimately, 5,301 people, most between the ages of 35 and 84, were recruited for the heart study. They all traveled to the Jackson Medical Mall, a formerly run-down shopping mall that was rejuvenated with a combination of health-care facilities and small retailers, for an in-depth interview and exam that lasted more than five hours and included scans of the heart, aorta, and abdomen. More than 85 percent returned for the next exam, about four years later, and 77 percent of the surviving original cohort came back for the next one. Those numbers are regarded as good to great, especially “for a group reputed to be difficult to recruit and impossible to retain,” says Taylor. “Trust was the key ingredient.”
To maintain that trust, study participants were represented on a host of important committees, including the ethics-advisory board and publications committee, where they were involved in decisions about the use of the data beyond the original study parameters and gave feedback on the public-health messages to come of the research. Allowing them a voice “reassures the community that at every turn, we’re thinking like they think,” says Taylor.
And with the long shadow of the Tuskegee experiment in mind, Taylor resolved never to keep helpful information from the participants. “I was a cardiologist before I was an epidemiologist,” he says. “Don’t sacrifice for methodological purity the right thing to do.” For example, since research has shown diet can help alter health outcomes, he gave that information to participants.
Participants also hear about published findings from the study — and there have been some notable ones. In what Taylor calls a “pleasant surprise,” researchers found that most of the study participants with hypertension managed it fairly well using medication. “That flies in the face of conventional wisdom that African-Americans tend to have vastly poorer control” of high blood pressure, he says. Still, the JHS found that participants 65 and older had about an 80 percent chance of having hypertension. “Having hypertension controlled is far better than not, but not having the disease is better,” says Taylor. He hopes to “aggressively try to figure out how to prevent” high blood pressure in the first place.
Research from the heart study also found that a large proportion of participants — 45 percent of women and 33 percent of men — had metabolic syndrome, a group of risk factors (such as a large waistline, a high triglyceride level, and a low “good” cholesterol level) that raise the risk of heart disease, stroke, and diabetes. The syndrome looked different in African-Americans than it did in European- and Mexican-Americans, with the JHS group more likely to have as a risk factor low levels of “good” cholesterol than elevated triglycerides.
Genetic analysis also is part of the study. While race is sometimes used as a proxy for genetic differences, it’s a poor one, says Taylor: “Genes are no respecters of racial boundaries.” Some 64 percent of JHS participants agreed to share their genetic information with other researchers via large international databases, says Jim Wilson, the study’s genetic coordinator and a professor of physiology and biophysics at the UMMC.
There’s greater genetic variability within an African population than a European one, says Wilson, because those who left the continent to populate Europe and elsewhere took only a small subset of the variations that existed at the time. So genetic information from African-Americans is a particularly rich field for searching not only for genetic variants that might confer risk for heart disease, but also for those that might be beneficial — such as one that occurs in a small percentage of African-Americans and actually protects against heart attack, says Wilson.
Heart-study participants contributed information that helped create the most accurate map of the human genome to date. Data from the study also led to the discovery of the molecular basis for the fact that a large percentage of African-Americans have a lower white-blood-cell count than European-Americans. (Though this finding doesn’t have direct implications for treating heart disease, the mutation that causes the lower white-blood-cell count is beneficial in Africa, because it protects people who carry two copies of the mutation from one type of malaria.) Another paper showed that genetic variants previously associated with progression of kidney disease in blacks also were tied to a significant increase in risk for atherosclerosis.
But while genetic information is helpful, potentially leading to the development of new drugs, for example, Taylor says genes are not always destiny, particularly with complicated diseases of the heart. Environment and lifestyle play a role. Scientists also are looking at the epigenome, chemical compounds that modify the genome and can be passed on from one generation to the next. Environmental and lifestyle factors such as stress, diet, and early childhood development may influence the epigenome. So all those factors, Taylor says, are just as crucial to study as genetics.
Taylor has known since early in his career that health was intricately connected with other socioeconomic factors. After an internship in Boston, he fulfilled his National Health Service Corps obligation by spending three years at a family health center in Liberty City, an inner-city neighborhood in Miami, whose patients came from many places: the Bahamas, Central America, Cuba, and Haiti. Taylor soon realized that care had to extend beyond the walls of the medical center, and that people had to become politically engaged to make their communities healthier places to live. He started a voter-registration drive from the health center and even wanted to ask patients whether they were voters and include that information in their charts. (That idea was vetoed by his superiors.)
The JHS collects socioeconomic data from its participants, and by analyzing that in conjunction with traditional risk factors, researchers can see that “some of the things in the social milieu get under the skin,” says Taylor. For example, it’s normal for blood pressure to drop at night. When that dip doesn’t occur, or is blunted, it’s associated with poorer health, including a greater risk of premature death. A JHS study found that even after accounting for other risk factors, people with lower incomes and less education were less likely to see a significant nighttime dip.
Mario Sims, a social epidemiologist and science officer in the heart study and an associate professor at the Mississippi medical center, was the lead author of a 2012 JHS paper that found people who perceived a lifetime of racial discrimination were 8 percent more likely to have hypertension than those who did not. (The study controlled for factors including socioeconomic status.) More recent, yet-to-be published work looks at perceived discrimination and behaviors like dietary, sleep, and smoking habits, says Sims.
“The study is really at a point of maturity,” says Taylor. “We’ve established it as a major platform for ongoing research.” In August 2013 it was funded for another five-year period, but NIH budgets have contracted, and no further rounds of medical exams are planned. Instead, the study will collect information from the participants’ hospitalizations, and researchers will continue to analyze the data that already has been amassed. And there are spinoff studies, such as one looking at whether yoga can affect risk factors for heart disease, that recruit JHS participants.
Sims says a logical step for the study is to move toward testing some of the hypotheses that have been generated. For example, while psychological ill-being seems to have negative effects on the health of African-Americans, positive factors like religious faith, optimism, and social support are hypothesized to protect against cardiovascular disease, says Sims. Because of this, interventions such as mindfulness and meditation might help. “We’re starting to collaborate with people so we can marshal evidence,” he says.
Though he has left Jackson, Taylor is not leaving his research on heart disease. At Morehouse, where he’s the new director of the Cardiovascular Research Institute and holds an endowed professorship, he wants to take approaches drawn from the heart study and other research and see if they can improve outcomes. “People are dying [of heart disease] at incredible rates,” he says. The DASH diet, for example, which focuses on vegetables and fruits, whole grains, and lean protein, isn’t widely adopted, but it’s been shown to be most effective among African-Americans, he notes. Observational studies have shown that three servings a day of whole grains are associated with a nearly 25 percent reduction in heart attacks, especially among African-Americans. Yet few people know what a whole grain is (it contains all the essential parts of the original grain seed), let alone what constitutes a serving (a half cup of cooked oatmeal or one slice of bread), he says. Moreover, research has shown the importance of exercise, yet few people meet the recommended levels. “The final frontier is behavior,” says Taylor.
He plans to explore new ways to help people change their habits, with possibilities including using digital technology such as mobile phones to disseminate information in accessible ways. Taylor is looking forward to working with scientists from other disciplines to encourage people, “as a part of how they live their daily lives, to make healthy options the default.” (He also plans to spend some time seeing patients, as he did in Jackson.) After tracking the trajectory of heart disease for the past 15 years, he’s ready to try to change it. “Observation is still critical, but there’s a lot we can do now,” he says.
Katherine Hobson ’94 is a freelance writer specializing in science and medicine.




No responses yet