Tackling antibiotic resistance one bug at a time
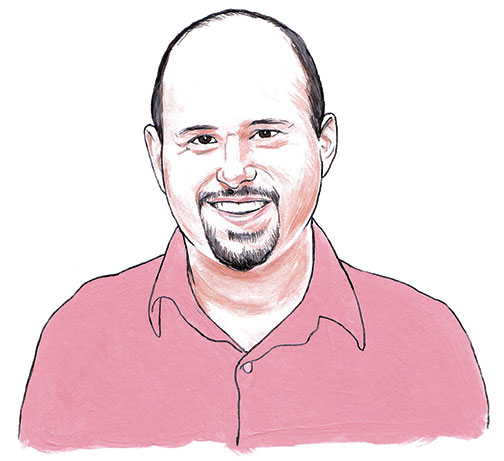
Pseudomonas aeruginosa is the bane of many hospitals. The rod-shaped bacterium has several skinny tails that help it to slink through catheters, water pipes, and our respiratory and urinary tracts, against the flow of moving liquids. “It can act like a bacterial salmon, moving upstream of flow,” Zemer Gitai says. This mobility allows it to colonize environments that are inaccessible to other surface-attaching bacteria, including the tissues and organs of those who have compromised immune systems, causing inflammation and sepsis.
In collaboration with Howard Stone, a Princeton professor of mechanical and aerospace engineering, Gitai’s lab has shown that these tails — called pili — act like hooks to pull the bacteria forward, resulting in a twitching, zigzag movement against liquid flow. The lab is trying to identify chemicals that can inhibit this unique motion. Rather than killing bacterial cells by targeting their ability to multiply, these drugs could block Pseudomonas from colonizing people’s bodies and hospital pipes, preventing infection. “If the bacteria does not have the capability to move through the hospital equipment or our tissues, we may be able to prevent people from getting sick,” Gitai says.
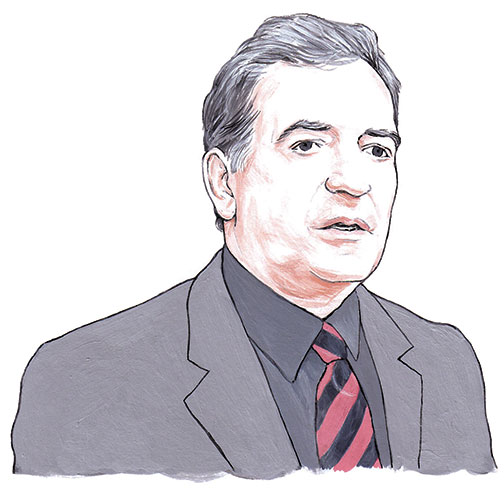
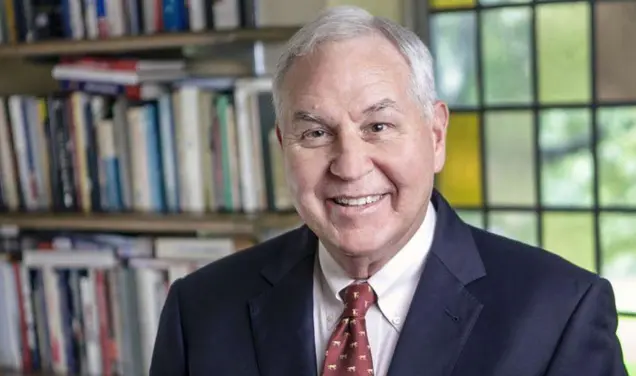
How do bacteria develop resistance in the real world? In the laboratory, bacteria are grown in test tubes and Petri dishes. But these environments do not necessarily mimic bacteria’s real-world habitats, which are complex and constantly changing. Robert Austin has developed a device that exposes bacteria to antibiotics in gradually increasing amounts rather than in a constant concentration, which more closely imitates true conditions. In an experiment with Princeton microbiologist Julia Bos, Austin found that E. coli that are gradually exposed to the antibiotic Cipro evolve resistance to the drug within 10 hours, or about 20 bacteria generations — much faster than under normal lab conditions.
Bos and Austin are working to understand exactly how resistance develops and spreads within the bacterial population. Low concentrations of antibiotics appear to speed up the emergence of antibiotic resistance, the scientists say. “There are a lot of tricks the bacteria have. They are more sophisticated than we thought,” Austin says.
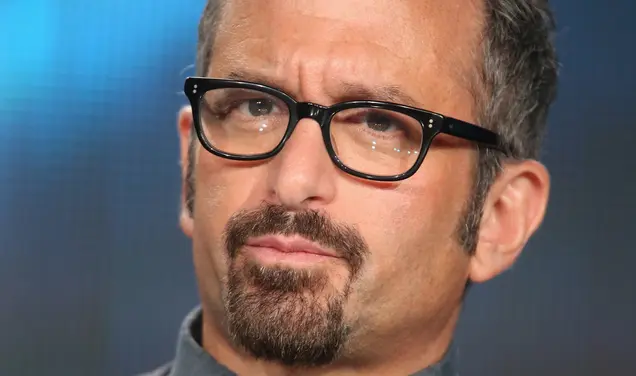
Mark Brynildsen is working to develop antibiotics that target bacteria more precisely. Existing antibiotics attack bacteria indiscriminately, which results in more rapid development of resistance. Brynildsen is working on an approach that would cripple only the bacteria in the host that are causing illness.
His lab also focuses on combating bacterial persistence, a type of hibernation state that allows bacteria to become tolerant or immune to antibiotics. “In the presence of antibiotics, persisters lie dormant for long periods of time, and when the antibiotic is removed, they wake up and re-populate the environment,” Brynildsen says. He is working to devise methods to identify these cells and find drugs to prevent their formation.











No responses yet