
Q&A: Dr. Celine Gounder ’97 on the Opioid Epidemic, Ebola, and More
PAW’s Q&A Podcast — June 2018
Celine Gounder ’97 started her Princeton career as an engineering student, but she eventually switched to molecular biology and found a calling in public health and epidemiology. In addition to practicing medicine, Gounder is a journalist and podcaster, and the current season of her podcast, In Sickness and In Health, explores the opioid overdose crisis. She spoke about opioids, as well as her experience as a volunteer during the Ebola epidemic in Guinea, in a recent interview with PAW.
This is part of a monthly series of interviews with alumni, faculty, and students. PAW podcasts are also available on iTunes — click here to subscribe.
TRANSCRIPT
Brett Tomlinson: I’m Brett Tomlinson, and welcome to the June edition of PAW’s Q&A podcast. Our guest this month is Dr. Celine Gounder ’97. She is an infectious disease specialist, and she’s also a journalist and podcaster who has written about a range of health topics. The current season of her podcast, In Sickness and In Health, explores the opioid crisis. Celine, thanks for joining me.
Celine Gounder ’97: Oh, it’s a pleasure.
BT: We have lots to talk about in your current work, but I’d like to begin with your Princeton story. Could you tell me a little bit about your undergrad experience, and how it’s influenced or informed the work that you do today?
CG: Yeah, sure Brett. So, as you said, I was Class of ’97, I started off, well I started at Princeton at the age of 16, I was very young when I started. And still trying to figure out what I wanted to do in life, and my father was from India, and sort of a typical tiger Asian parent, and he really wanted me to be the next Bill Gates. So he wanted me to study computer science, and engineering, and then go to business school, and go along that path. And you know, I started off as an engineer at Princeton, and I just couldn’t see myself in any of the jobs that that training was going to lead to. And for me, that was really frustrating. I didn’t really understand what I was doing, and why, and it just didn’t make a lot of sense to me.
And eventually, I ended up switching majors to molecular biology, still in the sciences. But to me it was about how could I use science to do something good for others in a way, I guess, that made sense to me? My parents were both from outside of the U.S. My father from India, as I mentioned, my mom grew up in France, in the aftermath of World War II, in Normandy. And so, I was always very aware of, you know, how privileged we were in terms of how we grew up here, and really wanted to find a way to give back. and you know, sort of — OK, I’m going to have you scratch a little bit of this, but how we could give back to the communities that we came from, as well as others who hadn’t had the same advantages as we did. So I did make that switch, and you know, it’s funny, one of the classes that really was perhaps one of the most formative was not in my major at all. It was a class in medical anthropology. We studied, for example, Paul Farmer and his — who’s a doctor who’s worked for decades now in Haiti, as well as other countries. And he talked about some of the issues around stigma in Haitians, and caring for patients with HIV, and how aid workers, international donors, didn’t all — while they wanted to do the right thing, oftentimes their efforts may have backfired with respect to the people they were trying to serve. And so, that really was quite formative.
And I think one of the other really important experiences for me was the Princeton thesis. And I think a lot of students approach that with dread. You know, this massive undertaking that you need to get through to graduate, and I think it’s actually an amazing opportunity to pursue something really important to you in a lot of depth, and in a way that could really shape your career later. And as part of my thesis research experience, I spent a summer at the World Health Organization in Geneva, and did a lot of my research with people there at the time, and then continued that work over the course of my senior year. And that really was how I started to understand global health and that that would probably be a big part of what I was going to do in my career later.
BT: And did you take a direct path from Princeton to medical school? Or were there stops along the way?
CG: Yeah, there were stops along the way. I finished Princeton, and I wasn’t 100 percent sure I wanted to go to medical school. I knew I wanted to do something with public health, and so, I took a couple steps, actually, along the way. The first was spending a year in Washington, D.C., working for Ralph Nader and Gordon Douglas, both Class of ’55, so this was part of Project ’55. And I was one of two from my class who were hired to help advocate for funding and programs for tuberculosis control overseas. And Ralph had said at the time, you know, why is it we see all this advocacy around HIV, but not around equally big killers globally, like tuberculosis? And that’s really where I started delving into that disease in particular, but also global health and policy more generally.
And then, during that year, I met a number of people in the field, and was sort of recruited to some degree to come to Hopkins, where I then spent the next two years doing a master’s in epidemiology. I spent some time in Brazil during that stretch, in the favelas and Rio, studying HIV and tuberculosis. And that really, again, was another really formative experience, it was a lot of the work I ended up doing for the next, over the next decade. And was a really long-term relationship with the folks at Hopkins. You know, so I wasn’t actually sure that I wanted to be a doctor until then, and I knew I wanted some involvement in public health, but it wasn’t until a bit later that I was sure that being a doctor was going to be part of that mix.
BT: And what was it that made you decide, you know, beyond the focus on global health, and public health, that you wanted to have that kind of interaction with individual patients as a doctor?
CG: Well I think it’s a few things. I think someone I was working with at the time actually put it really well, she said, “You don’t really understand disease if you don’t take care of patients.” And it’s only by really taking care of patients and owning their care on an individual level that you really understand. And I really bought into that idea, and what I realized actually is, as I went through medical training, and started to actually take care of patients on my own, that I really enjoyed it. It wasn’t just about understanding how the system worked, or how disease worked. I really liked taking care of people.
There’s a lot of different pieces to it. There’s being there for somebody at a really critical point in their life, there’s, you know, with an AIDS patient, for example, seeing them go from, you know, really cachectic, so skinny like you have cancer, to an overweight diabetic, they do so well. You know, you’re there at the bedside when they are at the end of their life, and they’re sort of coming to terms with things, and their family is, and it can be a really beautiful moment. And there’s also sort of the scientific challenge of figuring out what’s happening with people. It’s sort of a puzzle that you have to decode. And so all of those pieces are really fun.
BT: I gather that you volunteered as an aid worker during the Ebola epidemic in Guinea. Could you tell me a bit about how you went about doing that, and what that experience was like?
CG: Yeah. So you know, as you might remember, the epidemic started in December of 2013, and didn’t really hit the headlines here until the following summer. So, not until July. And I started seeing reports of the outbreak probably January, February, and actually started pitching some of the media I work with about the story. And at the time, they were like oh, that’s not a story, no one’s interested in that, that’s like Ebola in backwoods Africa, who cares about that? And probably around March, April is when I started to reach out to the World Health Organization, and then Médecins Sans Frontières, which is Doctors Without Borders, to see how I might be able to volunteer.
At the time, the WHO effort in Guinea, which is where the disease started, was pretty disorganized. And I had another friend who went over around that time, and it was pretty scary. The security situation, not just in terms of disease, but actually more so in terms of local populations attacking healthcare workers, was a major problem, especially in the beginning. And it just didn’t seem like government officials were really looking out for the safety of health workers who were coming to help. They really just wanted to cover themselves. And in terms of MSF, they were very quickly overwhelmed, as the disease started to ramp up over the course of May, June, and then July. And they had more than enough volunteers — the way they described it was that it doesn’t matter if you have lots of pilots and flight attendants, if you don’t have enough planes to fly, there’s not much for those pilots to do. And that was kind of the situation they were in. They didn’t have the infrastructure, the beds, the supplies, just the basics, to provide care.
And so, that’s when finally, some other agencies started to get involved, everyone from IRC to Partners in Health, to International Medical Corps, to a whole host of others. And so, I was reaching out to a number of them, and at the same time, contacted every single level-four biosafety lab, biosecurity lab, in the country, asking for training, because there is specialized training for how do you treat Ebola patients, and sort of the infection control issues around that. And then that’s when finally, somebody who I contacted at one of these level-four labs gets back to me and says, you know, CDC is starting to organize something around this, they’re actually getting a lot of us together to offer their own course for people who will be going over. So I enrolled in that course, and around that time also, got a — was offered the opportunity to go over with International Medical Corps to Guinea. So Guinea is where the disease started, and then it looped back around to Guinea later in the epidemic. And what was unique about that was, it’s a French-speaking country, so many of the volunteers, especially from the U.S., obviously, were English-speaking, and they really needed people who could speak French, and who had the medical and public health background. So, as a French speaker, it was a good fit.
So when I finally went over, at that time, it was already starting to fade from view in the U.S. A lot of our attention was driven by, you’ll remember there was a doctor by the name of Kent Brantly who became infected, he was brought back to Atlanta for treatment, and then we had a couple other, handful of other healthcare workers. The last of whom was Craig Spencer, who was brought to Bellevue Hospital in New York for treatment, and basically after he was released from the hospital, after our midterm elections were over — and our elections also drove a lot of the political discourse around Ebola, you might remember Governor Cuomo in New York, and Chris Christie in New Jersey, you know, a lot of what they were saying at the time about quarantines, and travel bans, and all that kind of thing — by the time I went over, it was already fading from view, which is really interesting because we were in an especially precarious situation in West Africa at that time. They were starting to really bring things under control in Liberia and Sierra Leone, but the disease was threatening to spread back into Guinea, and into their capital, Conakry, which is bigger than the capitals of Liberia and Sierra Leone. So a really dangerous situation. And fortunately, a lot of the work we were doing, in terms of gearing up hospitals to be prepared for this, and improving the situation in the community around their public health practices, that really prevented a catastrophe from happening in Guinea. But, you know, we did continue to see cases, and you know, it was really an amazing experience to be part of working alongside people there.
BT: You have these various skills in public health and as a physician, to have a tremendous impact on lives. But you also seem very driven to reach a wider audience in the work you’re doing as a journalist, and as a documentarian. Where does that part of your professional life come from, and is that something that’s kind of always been there? Has it developed over time?
CG: Well, I think it has developed over time. My husband, who’s Class of ’96, but a very different kind of journalist. He started off at Sports Illustrated, actually right out of college, and so I’ve been exposed to the profession, and learned a lot by osmosis, but it wasn’t something I had directly considered until later, and it was really because of what I was seeing.
Working in sub-Saharan Africa, in Soweto, for example, in South Africa, and doing research, getting grants, publishing papers, all of that was going well. But then I was sort of asking myself what impact are we really having to help people on the ground? I felt like it was more of a factory for churning out academic products. And I found that really frustrating. And I also felt like, in my clinical work, even in the U.S., I would see things that the broader public just doesn’t know, doesn’t understand, and it’s hard as an outsider to the profession to really understand how medicine works in a lot of ways — the culture of it. And I really felt like there are problems in our system, and giving light to some of those issues is the only way to help bring about change.
BT: And the complexity of the issues seems to lend itself well to the type of podcast that you’re doing, In Sickness and in Health is this very detailed, very well reported, comprehensive exploration of an issue. The first season being youth and mental health, and then currently the opioid overdose crisis. Which seems to be kind of the overwhelming public health story in the country right now. Why did you choose this particular topic, and what sorts of things are you learning that maybe were new, even to you, before you began reporting this piece?
CG: Well, you know, because of what I do for a living, taking care of patients with HIV, a lot of my patients do use drugs. That’s how they end up getting HIV in the first place, very often injection drug use. So it’s something I have had a lot of experience with in my own patient population, but over the course of my medical training, I saw what happened with prescription drugs, with the Purdue Pharma oxycontin story. I saw that patients were switching to heroin, I saw patients then overdosing from fentanyl in the last few years. So it’s something I very much saw in my own practice, and I saw it emerging as a major problem.
Also, as an infectious disease provider, there are a lot of complications of it. You know, heart infections, and bone infections, related to drug use that you see, that were spiking. But, and this actually refers to some research by two Princeton professors, Anne Case [*88] and Angus Deaton, who a couple years ago, published a paper looking at the decrease in life expectancy among Americans, and a lot of that is we’re seeing an increase in deaths among middle-aged Americans, and much of that is driven by the opioid epidemic: overdoses and complications of drug use. And it really is the public health problem in the U.S. today.
BT: And you’re exploring it from many angles. I mean, the psychology and the physiology of addiction, but also, the criminal justice system, and the history of race in America, and also, these many individual stories. From a reporting perspective, how do you kind of keep all these threads, you know, together and coming together into the same story? How do you approach the project, and how do you kind of organize it in the reporting that you’re doing?
CG: Yeah. You know, I don’t think of myself as an investigative journalist. I think that’s really best left to people outside of the profession, because it does involve a certain confrontational, attacking sort of stance, so to speak. I think of myself much more as somebody within the profession who’s attesting to the issues I see among my patients, and looking at what the science says, in terms of how we can help people. And so, I started off the season, as you say, talking about the neurobiology of addiction, and how people, and why people become addicted to drugs, and what that really means. And then I move onto other issues, including some of the programs that have been studied to help people with addiction, including law enforcement assisted diversion, away from jail and prison, to housing and treatment programs, like they’re doing in Seattle, or what’s called safer injection sites, or supervised consumption sites, where people are given a safe place to use their drugs, not in public, so not in the park, not in a McDonald’s bathroom, where you have people who can monitor and make sure they stay safe, and have clean equipment. And these are things that, for a lot of people, you know, who aren’t familiar with the problem, it might sound crazy, and so you really have to talk them through an individual patient story and help them see why it works, and that this is actually about helping people get treatment, and get them into the medical system.
And so that’s how I really do approach it. I think the final part of what I’m trying to address with the series is sort of more what the social sciences can bring to the table. Whether that’s history and anthropology, and understanding why our views about drug use and addiction are so different actually in the U.S., compared to the rest of the developed world. And that really does have very real implications for the trajectory of the epidemic. No other developed country is dealing with a problem like ours right now. It’s really quite unique to the U.S. And you really can’t address it without looking at what about our history is different. So, I try to think about it in those terms: You know, the individual patient, and science, and the public health population level approaches we need to take.
BT: And in terms of policy and programs, are we making progress on this epidemic? Is it noticeably different today than it was six months, or a year, or two years ago?
CG: Gosh, I wish this were not the case: I think it’s going to get worse before it gets better. So, what we’ve seen as a progression from prescription opioids, so drugs like Oxycontin, Vicodin, Percocet, to heroin, and now heroin is contaminated, adulterated, with fentanyl, which is a synthetic opioid which is many times stronger, and people don’t know really how strong the drug they’re taking is, and if it has fentanyl in it or not. And so they can’t really gauge how much to use when they use, and so the rates of overdoses as a result are skyrocketing.
And you know, once somebody’s dead, the game is over. You can’t get them into treatment anymore. There is no hope anymore. And so, if we really want to be helping people, we first need to address the fentanyl overdose issue. Some people might say that’s enabling. There are parts of the country, they talk about three strikes, you’re out. Well, you know, what if that person was somebody who, after four overdoses, they actually got into treatment and turned things around? You know, who’s to say when that’s going to happen for somebody? It’s not really for us to play God and judge.
So, I wish I could say things were going to turn around sooner. There are some things that are great. Some cities are taking some very innovative but science-based approaches, things that have been proven elsewhere, in other parts of the world, whether it’s Vancouver, or Sydney, Australia, or Geneva, or in Britain. They’re adopting some of those approaches here in the U.S., be it Seattle, or New York, or Boston, Philly, Baltimore. There are some rays of hope in that they are trying to be more proactive about saving lives, getting people into treatment. But it’s sort of one step forward, one step back. You also have discussion of ramping up the law-and-order, tough-on-crime approach. So it’s hard to know which impulse is going to win out here. And it’ll probably be different in different parts of the country. And that kind of amounts to a natural experiment as to what’ll work, and what won’t.
BT: And do you think the people in the medical professions are being heard in this conversation? I mean, as policy makers begin to make those decisions on the local level, or the state level, or nationally, are they listening to what the folks who are kind of on the front lines have to say about this?
CG: I think they are to some degree. But you have to remember, you know, doctors don’t practice in a vacuum. They’re also very much a part of their own community, and they share many of the same values and culture as their own community. So, on the one hand yes, you are witnessing something a bit different from your neighbor, who’s not a doctor, and you’re caring for patients in a way that others aren’t. But it’s not so straightforward that these reactions are completely science-based for anybody, including myself.
Do I think doctors are being listened to though? I think more than they have in the past, I think law enforcement has really dominated the conversation, and I think the fact that doctors and public health workers are more and more a part of the conversation is helping change the direction of where we’re headed.
BT: You have taken this deep dive into journalism, but you also remain a practicing physician. Do you see yourself continuing this sort of dual track, or multitrack career?
CG: I do. I mean. it is challenging to balance the two. Not just logistically and in terms of time, but there are conflicts of interest that you have to navigate.
The way I look at it is really about what I bear witness to as being problems in how our health system works, the kinds of issues my patients deal with, and how can we better understand those and tackle those, as opposed to reporting on laying blame at the foot of a particular person, or company, or hospital system.
It is part of how I also process what I see. I think you see a lot of burnout among physicians now, and I think being able to share what we see and experience with others, and be able to make a difference not just in the exam room,at that level, but to be able to make a difference in terms of how people think about problems. I think some of the nicest compliments I’ve gotten on the podcast have been, “Gosh, after I heard that episode, I treat my patients with this problem in a different way,” or “I’ve started doing this, and I never did that before.” Or, “I have a friend who has an issue with addiction, and I just didn’t get certain things about it before, and now I understand, how I can be more helpful or not.”
Being able to change the way people think is really important to me. I think you can have a broader impact in that way.
BT: Well it certainly sounds very rewarding. Celine, thank you so much for joining me. This has been great.
CG: Oh, well thank you for having me, Brett. It’s really been a pleasure.
BT: Celine Gounder’s podcast is In Sickness and in Health. You can find it on iTunes and SoundCloud, on its website, insicknessandinhealthpodcast.com, or on Twitter, @isihpodcast. Celine is on Twitter as well, @celinegounder.
If you’ve enjoyed this episode, we invite you to check out our archive and subscribe in iTunes to hear more interviews with Princeton alumni, faculty, and students. Princeton Alumni Weekly is an editorially independent magazine by alumni for alumni since 1900. The music in this podcast is licensed from FirstCom Music.
Paw in print
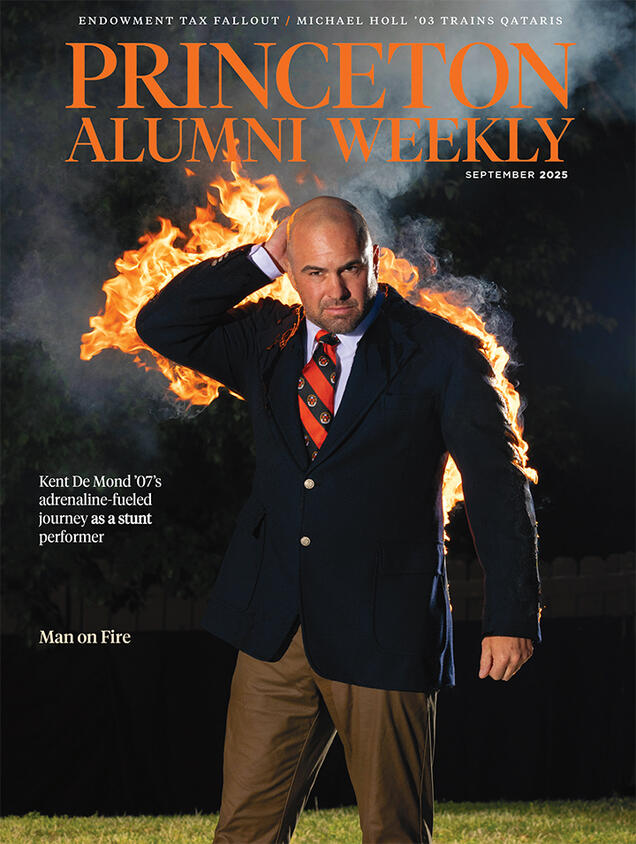
September 2025
Stuntman Kent De Mond ’07 is on fire; Endowment tax fallout; Pilot Michael Holl ’03 trains Qataris

No responses yet