
“He’s looking right at me,” says Dr. Yolandra Gomez Toya ’88 as she reassures the mother of 6-month-old Regis Toledo that the infant is developing just as he should. The chubby-cheeked, brown-eyed boy has no clue that his pediatrician is unusual, but she is. Toya’s heritage is Native American.
Of the approximately 956,000 doctors in the United States, just 3,475 are Native American, about one-third of 1 percent. (The most recent data are from 2013.) The nation’s 6.6 million American Indians and Alaska Natives (the two groups are generally combined) make up about 2 percent of the total U.S. population. As for the number of pediatricians like Toya, “the picture the data paints is not a great one,” says Dr. Shaquita Bell, chair of the Committee on Native American Child Health of the American Academy of Pediatrics. Fewer than 300 pediatricians, about half of 1 percent of all pediatricians in the country, are American Indian.
Toya is examining little Regis at a clinic at Jemez Pueblo in New Mexico. The 51-year-old doctor drives 32 miles to this tiny community twice a month, on her days off from a full-time job at a pediatrics practice outside Albuquerque. More than half the pueblo’s 3,400 members live in the village nestled in a valley bordered by red sandstone cliffs. Toya’s husband was raised here. When her colleagues ask why she doesn’t play golf or ride a bike on her time off, Toya is emphatic: Native American communities “need our help, because there’s so much work to be done to make those communities healthy.”
While there are few Indian doctors, there are plenty of problems to treat. One national study found 4-year-old Native American children are twice as likely as other children to be obese. Those aged 10 to 19 are nine times more likely to be diagnosed with Type 2 diabetes. Native teens have the highest rates of suicide and teen pregnancy of any population group in the United States. Poverty rates are higher for Native Americans than any other racial group.
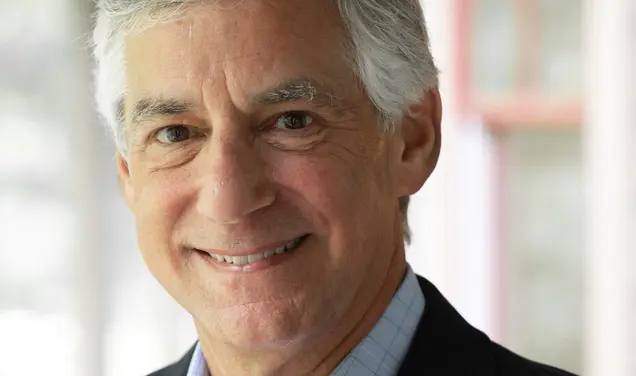
Dr. Donald Warne, a member of the Oglala Lakota tribe and chair of the Department of Public Health at North Dakota State University, believes training more Native doctors and other health care professionals will improve the quality of care for American Indians. “The low-hanging fruit is to develop our health-care workforce in Indian country,” he says. Toya agrees that this could have a positive effect on health, describing her work as “rolling up my sleeves and working on the front lines in a Native community.”
Growing up poor in rural Dulce, N.M., Toya dreamed about being a doctor. Born Yolandra Gomez to a Jicarilla Apache mother and Hispanic father, she was the ninth of 10 children. They were sheep-and-cattle herders whose nomadic lifestyle entailed spending much of the year in a ramshackle two-room home that lacked plumbing and electricity. “We always had an outhouse,” Toya says. Wood gathered, chopped, and stacked by the children was the primary source of fuel. Lambing season brought a chance to play doctor. “Some of the lambs were too sick to nurse so we would take the lambs [to be fed], and that became our full-time job.” The children learned to butcher, too, which sparked Toya’s interest in biology.
Sheep were — and still are — an important source of food for the family. Preparing for the annual Jicarilla Apache feast day known as Go-Jii-Yah in mid-September, Toya’s mother, Cora Gomez, and her sister, Michelle Gomez, have slaughtered two animals. The feast day is a harvest celebration when tribe members flock to the shores of Stone Lake on their northern New Mexico reservation, camping in dome tents, RVs, and traditional teepees. The family’s 87-year-old matriarch watches her adult children as they cut meat from the lambs’ bones and slice potatoes, carrots, and celery. Toya pats dough for fry bread and slides it into a cast-iron pot of bubbling oil. Fry bread isn’t part of a traditional Native diet — it was first made when the U.S. government offered American Indians rations of free white flour, lard, and baking powder. Toya knows the crispy, plate-sized rounds drizzled with honey aren’t healthy, but they’re irresistible.
As the stew simmers in huge pots on a cast-iron grate over a wood-fired stove, people prepare for a relay race between the tribe’s two clans. Many retreat to circular kivas constructed from aspen branches to be blessed by medicine men. Four white circles painted on their faces symbolize the Earth, the sky, the sun, and the moon.
It is a ceremony far removed from Princeton, nearly 2,000 miles east. In sixth grade, Toya spotted a photograph of Princeton’s ivy-covered stone buildings and told her teacher she wanted to attend the University someday. “You can’t go there,” he told her. “Only rich, white, smart people go there.” But Toya thought, “I know I am at least one of those things.” Five years later, a family connection led her to Alfred Bush, then the curator of Western Americana at Firestone Library. He encouraged her to apply to a boarding school in Colorado for her senior year of high school and then to Princeton. Once admitted, Bush paid her way to visit.
Bush chauffeured Toya to and from Newark Airport, and hosted dinners where he introduced her to Native American and Latino students. There were fewer than a dozen American Indian students at the time, according to Bush, and they came from different tribes with little in common. Bush wanted to be sure “they stuck around, and most of them did,” including Toya. A Woodrow Wilson School major, she went on to the University of California, Berkeley, for a master’s degree in public health and to the University of New Mexico School of Medicine.
At UNM, anatomy class presented an early challenge. When a Jicarilla Apache died, Toya explains, “traditionally that body was put away immediately. It was wrapped and put up in the mountains somewhere in the ravine, and everything was burned. ... The house was burned; all their belongings were burned.” Medical students are assigned a body for a semester to dissect weekly, but many Native cultures discourage touching dead bodies. When Toya consulted tribal medicine men for advice, they initially urged against her participation. Toya worked with them to develop blessings to protect her from the spirits with “strong medicine” consisting of “smudging or smoking” herself — part of a purifying ceremony — and chewing special roots. At the end of the semester, she prayed, cleansed herself, and made an offering to the cadaver so that the “spirit could rest.”
Since Toya’s time at UNM, the university has changed its curriculum, says Dr. Gayle Dine’Chacon, a Navajo who founded and directed the school’s Center for Native American Health. Students who don’t want to be in the room during autopsies are permitted to view them on a television screen outside.
Bell, of the American Academy of Pediatrics, faced a different conundrum during her medical school years. She was told to cut her hair because it might get in the way during a procedure or touch a patient. Trimming her long locks violated her Cherokee beliefs. “We cut hair for really major events — so birth, death, weddings,” Bell says. “Your hair basically holds those memories.” She took the issue to supervisors, who allowed her to keep her hair and her tribal identity.
Now, Bell guides others who confront cultural disparities. Some Indian students come to the classroom at a disadvantage, she says, since medical school tends to employ a “lecture-style, competitive, grade-based situation.” That’s very different from Native American teaching, which she described as “supporting each other and not to put yourself ahead.”
Toya mentors students, too. She believes the biggest obstacle for Native students is getting admitted to medical school in the first place. Of the 19,254 graduates in 2017, just 30 were Native American. Many just “don’t understand the rules of the game,” Toya says, and need a guide to help them through the process, “somebody who sits down with them, emails them, texts them. Did you do this? Are you signing up for chemistry? Did you take that summer class?”
Toya has been offering that kind of advice to Erica Charley for years. Charley, who grew up on the Navajo reservation spanning New Mexico, Arizona, and Utah, where unemployment tops 40 percent, didn’t think she’d graduate from high school, let alone become a doctor: “Coming from nothing ... you feel downtrodden.” Toya encouraged her along the way and taught her techniques, including suturing lessons using pigs’ feet. Now a first-year surgical resident who aims to be a transplant surgeon, Charley still shadows Toya and is a mentor to medical students herself.
Young aspiring Native doctors often live on reservations in remote locations with little or no access to the internet. They’re more likely to confront financial hurdles. The average debt for all graduating physicians in 2016 was $190,000, according to the Association of American Medical Colleges — and that doesn’t count undergraduate loans. For many, those daunting figures would rule out medical school, says Bell: “To somebody who had no running water growing up, that is astronomical, it’s unfathomable.”
Toya’s family couldn’t bankroll her education, but she was lucky. Princeton offered her aid, and her tribe helped, too, paying for most of her education. In 1887, the U.S. government granted Jicarilla Apaches a reservation that sits on the Continental Divide. Toya’s great-grandfather helped negotiate the deal, riding to Washington, D.C., in a cattle car (Native Americans were prohibited from riding in the passenger compartments). In the 1950s, oil and gas were discovered on the land, and royalties now fund scholarships. Not all tribes have such resources, but the Indian Health Service offers scholarships, as do the Association of American Indian Physicians and other organizations.
At Oregon Health and Science University, Dr. Erik Brodt is on a mission to boost the number of American Indian health-care providers. Brodt, a member of the Ojibwe (or Chippewa) people, started the Northwest Center for Native American Excellence and hired 12 full-time Native American faculty members to help reach Native youth. There were only 194 Indian medical-school faculty members nationwide in 2016, and just eight of the nation’s 143 medical schools educate half of all Native American doctors, according to Brodt.
Family practitioner Dr. Dan St. Arnold, also Ojibwe, has similar goals. He lauds programs to reach potential medical students sooner, and points to one led by the American Academy of Indian Physicians. The weeklong summer trip brings 25 Native high school students to Washington, D.C., each year to meet health professionals. But despite programs and scholarships, the number of Indian applicants to medical school has plateaued, puzzling him.
St. Arnold attended the Jicarilla Apache feast day, sitting in a lawn chair on the sidelines of the relay race. His wife, a Jicarilla Apache, is Toya’s cousin. St. Arnold spent 25 years working with the Indian Health Service, which paid for his medical education; he argues that diversity in health-care professions improves outcomes for everyone. “Studies have shown that people — whether Native American, African American, Asian, even white Americans — respond better because they’ve experienced what you’ve experienced,” says St. Arnold. “The best care comes from people who know where you’re coming from.”
St. Arnold and Toya served together on the admissions committee at UNM’s medical school a few years ago. Even in a state with a large Native American population (about 10 percent), Toya saw evidence of racism. “You’d hear people say things like, Native American kids aren’t smart enough. They can’t cut it.” St. Arnold suggested that admission officials focus not on “grades, but look at the road [the applicants] had to follow to get to that point.” Racial bias doesn’t end after students graduate from medical school: When Toya was a senior resident working in a neonatal intensive-care unit and wearing her green scrubs and stethoscope, a white nurse once assumed she was a janitor and asked her to plunge a toilet. Toya reported the incident because she wanted “that nurse to understand that, you know, not all of us brown people are the janitors.” Students still bring her similar stories, she says.
Back at Jemez Pueblo, parents appreciate Toya’s dedication. When 7-year-old Tahi Toya (no relation to Yolandra) was diagnosed with acute flaccid myelitis, a rare condition that affects the nervous system, his mother sought advice from both a medicine man and a team of doctors including Toya. The viral-induced illness doesn’t have an effective treatment. A month-long healing ceremony at the pueblo helped, according to Tahi’s mother, Tricia Toya, who added that Yolandra Toya respected “the values Natives have” and understood the family’s need to turn to “different ways of belief to look for answers.”
Toya also volunteers at Jemez on evenings and weekends. She urges parents to feed children more fruits and vegetables and to get them to bed earlier. She acknowledges that this is tough for families with incomes below the poverty level and whose homes consist of a couple of rooms for multiple generations. She’s the first physician at Jemez to participate on a family-support team aimed at identifying and helping children with learning and behavioral problems. And she’s embarking on a new project with the American Lung Association to diagnose and treat asthma. The disease is prevalent in places like Jemez where wood stoves are used for heating.
Just being a presence on the pueblo is generating results. “I can make the biggest difference in their lives if they see me as a Native American woman physician who cares about them,” she says. On one home visit, she spotted children playing doctor. She beamed and reported, “All the little girls wanted to be Dr. Toya. My job is done!”
There’s success on a personal level, too. Her daughter Anya, a junior at the University of New Mexico, plans to apply to medical or dental school. She, too, may be Dr. Toya someday, the first female physician who is Jemez.
Kathleen McCleery ’75 is special correspondent and freelance producer for PBS NewsHour.







No responses yet