
I’m Liz Daugherty, and this is the Princeton Alumni Weekly’s PAWcast, where we talk with Princetonians about what’s happening on campus and beyond. Today’s episode was recorded at Princeton University’s 2024 Reunions Weekend, when PAW sponsored a panel discussion featuring five alumni experts who addressed two questions: Is student mental health in crisis, and what can be done about it? The conversation begins with moderator Dr. Lucy McBride, Class of 1995.
Listen on Apple Podcasts • Google Podcasts • Spotify • Soundcloud
Lucy McBride ’95: Thank you so much for the introduction and thank you all for being here and I’m really thrilled and honored as a proud Princetonian to be here to talk about mental health. I think it’s relevant, it’s in the news and it lives in our everyday lives. And so I just wanted to talk first briefly about the goals of this panel. The goal here is really to have a collaborative dialogue with you guys. I think as we all know, mental health is a process, it’s not an outcome. And in that spirit we’d like this to be first a talk, each of us will speak and then we’re going to open it up for discussion. So half of this conversation will be us talking, but we do not need to clog the airwaves with all of our mental musings and ideas, even though we could, because the five of us combined have a lot to say about mental health.
I also want to say that we have humility about what we don’t know. We have perspectives, we have a lot of collective experience, but we cannot speak for anybody else, ergo, this is a conversation. It’s also designed to remind everybody here and whoever’s listening that we’re not alone. Mental health is, guess what, part of the human condition. The question isn’t do you have mental health, the question is what are you doing about it and how honest are you about your own mental health? And then how are you conceptualizing mental health in your whole health, in your family, in your community?
So we’ll get started and I’ll start by welcoming you again and telling you that there are five of us here, each of us who have a different perspective on mental health. We come from various disciplines and perspectives, and I’m not going to bore you with our bios because those are written out for the distinct purpose of us talking about the meat and the flesh of what we’re going to get into.
So the title of this talk is provocative intentionally. It’s a question. Student mental health, is it a crisis and what should we do about it? So let’s start there. When we met as a group on Zoom — which was by the way, one of the more fun hours of my spring or year, these people are new friends and mentors — we talked about, is it a crisis? This is an open question. Is it overblown or are we not talking about it enough? And we came to the conclusion that there is no conclusion. That the question itself matters and we came to the conclusion that it’s distinctly not a calamity. There is hope. It’s not a calamity. Is it a crisis? Is it an uppercase C? Is it a lowercase C? I think we can agree that it is a crisis, lowercase C, but the semantics almost don’t matter because when we’re talking about mental health, what we’re really talking about is health.
And that’s where we agree, that in so far as mental health is an issue in people’s personal lives, family lives, communities, and on college campuses, it’s actually a health crisis. So mental health is health. It’s not just a hashtag. It’s not just a cute staying. It’s not a bumper sticker. Mental health is health. If we define, as I do with my own patients and in my writing, health as the integrated sum of our behavioral, physical, soc-emotional, and spiritual health, when mental health is on the fritz or in the balance or in peril, every aspect of our health is at stake. As a primary care doctor seeing patients for 20 years, I can tell you that every single patient of mine has mental health, whether he or she knows it or not. I have mental health. In fact, it was at this university where I realized for the first time I had mental health. I had thoughts, feelings, and behaviors that were confusing and I didn’t have a vocabulary to name.
But in my experience seeing patients and talking about mental health, it’s become clear this is a universal health condition that we have mental health. So the question is relevant. What is health? What is mental health? And are they not inexplicably connected?
It’s also relevant because mental health is in the news. We’re hearing a lot of headlines from Jonathan Haidt’s new book, The Anxious Generation, to Jeremy’s book on loneliness, to fear-based headlines about how we are all going to hell in a handbasket. There is a lot of messaging about mental health and there should be. Mental health, as I just said, is part of the human condition, it’s part of our everyday existence and it affects everybody’s lives. So whether you are an alum, whether you’re a student, you’re faculty, you’re staff, you’re a panelist here, you have to acknowledge, in my opinion, that how you think, feel and behave and how you relate to other people and to alcohol, substances, food, Princeton, is relevant to your entire health. So I think there has to come with the question, some honesty about the fact that we all own mental health and then to name it.
So when we met as a group we decided that the question was relevant in itself, and then we did define health as the sum total of our mental, physical, spiritual, and behavioral health. And so today we’re going to offer some perspectives, hopefully not hand wringing, but rather some hope about what could be done with humility for the fact that we do not have the answers. So I’m going to go panelist by panelist and ask each one in no more than two or three minutes, tell me your perspective if you will: In what ways are we in a health crisis, if we’re going to call it that? And how do you see it from your vantage point? And we’ll go from Jeremy all the way down. Shoot.
Jeremy Nobel ’77: Well, thanks for that great opening and it’s great to be here with folks. I’m Jeremy Nobel and the full bio is here, but I’m internal medicine physician, public health practitioner, and a poet. And all of these have given me a perspective on mental health, what it is and what it’s not. And as far as this being a crisis, it’s certainly an accelerating urgency. If you have 60% of teenage girls being persistently sad and hopeless, that’s urgent to address. If you have suicide rates doubling over 10 years, that’s urgent to address. So there’s clearly an accelerating urgency and the question is in my mind as I think about is it a crisis, do we have the resources and insights to deal with it? If we do in public health, that’s called an urgency and you mobilize effort to address it. But you reserve “crisis” for something where you don’t have the resources, don’t know what to do and so on — I don’t think we’re quite there. And I think that’s something we should feel hopeful about, not go to sleep on, but feel hopeful about.
So the area of mental health that got my attention about 10 years ago was loneliness, which now is on many people’s minds and we think about it, the pandemic certainly shined a light on it. But it’s been accelerating for quite a while. And it’s also important to note that loneliness is not the same thing as being alone. Being alone is objective. You can measure the number of social contacts you have. Loneliness is the gap between the social connections you want to have, aspire to, sometimes dream about, and what you experience. And the growing amount of loneliness and the kind of, not just social but almost, and you talk about spiritual health, does my life have meaning and purpose? It disconnects you from a sense that my life has consequence.
This feeling of loneliness is probably the biggest preventable risk factor for depression, anxiety, addiction, and suicidality. So we do have things to feel urgent about, but we know what can connect us. We’ll talk more about that. But just to kick things off, just to let you know that I think it is an accelerating crisis: I think loneliness is the driver of what most people think about of mental health is the acceleration of anxiety. That’s Jonathan Haidt’s book. That’s what most people are experiencing when they say a sense of despair. It’s not schizoaffective disorder, bipolar disorder, borderline personality disorder, or manic depressive disease. It’s how we feel.
So the good news is we can shape how we feel both individually, in community and in culture. So that’s why I think we’ve got work to do.
LMB: Joshua?
Joshua Blum ’02: So my name is Joshua Blum. I’m a child and adolescent and adult psychiatrist. I work primarily in two universities, Bucknell University and Susquehanna University in central Pennsylvania. So this is essentially the work I do each work day. And I guess one thing I would say: I’ve noticed over the past several years that the trends on campus have increasing anxiety, increasing mental health needs, which we’ve not been able to meet. But I would say that yes, I think it’s a crisis, but nationally, perhaps internationally, but at least nationally it mirrors the same trends. So if you look at data, you can go on the CDC website and you can look this up yourself and you can see mental health trends over the last number of years. They’re not particularly encouraging. So the issues I think we’re seeing with college students really are not that different from issues that we see with other age demographics.
So I think that the issues we’re going to be talking about are probably symptomatic and more societal issues as a whole. What I specifically see with my patients would be a fair amount of anxiety, unsurprisingly, generally obsessive compulsive kind of things, trauma, quite a bit of that, depression, disordered eating, attention issues. A lot of pressure I think coming from a variety of sources. People feeling the need to do many, many, many, many things with the hope that they’ll be able to get a job afterwards, find fulfillment in various ways. Some of that might be internal, some of them may be from parents, societies at whole, I’m not really sure. Also a lot of anxiety about life after graduation. So where I work just recently had our graduations, and so I was talking to so many seniors about these issues, so many folks being very, very anxious about, “what’s going to happen after I graduate?”
Obviously, this is not a new issue. And I often tell them, go back in the past and watch some movies. Watch The Graduate, Dustin Hoffman, like who’s Dustin Hoffman? Watch Say Anything with John Cusack they’re like, who’s John Cusack? But I was like, you’re getting pressure from many people, family and so forth, to figure it all out. Guess what? Your parents didn’t know either.
But I think the thing that is a little bit different for the students that are going to be graduating and entering the workforce or going onto whatever they’re doing is sort of the pervasiveness of the information that’s out there. The inability to escape from 24/7 news. When I sometimes mention CNN 24/7 news, that was not necessarily a thing that all generations had to deal with. They’re like really? When you go on social media, Facebook or Twitter or whatever, they just kind of numb their brain or escape, they’re often going on there for totally other reasons, but they’re finding other things, care about this, outrage, all these other things that they didn’t necessarily go looking for. And so it’s no escape.
And so that’s a little bit different. And I think my wife and I, my family, we live in a university town. We live where I work, so we often talk with professors who are the people working in these places and they’re overwhelmed too. They don’t know what to do because it’s not that they just have to teach their subject now. They often spend a high amount of time counseling students about things they don’t feel prepared to do. Trying to accommodate students in various ways. That’s not necessarily new, but then the after hours, what do I do about this aspect of my family, this aspect of my mental health is now pervading and affecting my schoolwork. And they’re like, we don’t feel trained for this. So I think that’s a little bit different as well.
LMB: Chioma, congratulations on graduating in the Class of 2024.
Chioma Ugwonali ’24: Thank you, Lucy. Yes. So I’ll be sharing a perspective as a senior who is really involved with different mental health projects and committees during my time at Princeton. From my perspective, I would say that youth, we’re really fluent in the language of mental health. We know how to talk about how we are feeling. We understand that this is an issue. We know the problem, we don’t know the solution. We don’t know how, well, actually, I’ll take that back. I feel like we do. I feel like we do, but it’s harder than simply having more counselors or having a group discussion session or even just hosting painting sessions, which I love doing. But they seem almost superficial sometimes and sometimes Band-Aid solutions to the root issues of loneliness, of overwhelm about what is coming next in our careers.
And particularly here at Princeton I’ve heard from a lot of students, myself included, feel this anxiety and stress about how to live up to the Princeton name because we see and we meet all these amazing alumni, they’re doing incredible things. And each of us feel like in some way, shape or form, how can we be that next Sonia Sotomayor [’76] or Michelle Obama [’85] or et cetera, et cetera. And it’s a lot of pressure. It is potentially self-inflicted to an extent, and it’s not necessarily a bad thing per se, but when it becomes your whole life and you have all these different voices, sometimes from your family, from friends, et cetera, telling you that this is what you need to do, it’s overwhelming. And I find a lot of students — and I’m also a RCA, I don’t know if I put that on here, but a residential college adviser or RA for two years. And so I hear from my students, their first step on campus they’re wondering, what are the right classes I need to take so that I can have this career? And it comes to an extent where we’re going down these well-defined paths and we don’t even really feel like we know what we’re doing, why we’re doing what we’re doing.
And so to this potential mental health crisis, I would add a sense of purpose, a missing lack of purpose sometimes and guidance and direction and reflection. And that spiritual connection that I’m sure we’ll talk about more, having a sense that you’re related or connected to something higher than you, that even if when you do make mistakes, there is a better, a greater plan in mind and belonging undergirds all that. Having this feeling that there are people who are looking out for you and who are invested and want to see you thrive. Not just survive, because there’s this conversation about the grind here at Princeton and other campuses: “Oh, I just have to get through this exam. Well, I have to just get through this class.” But it doesn’t have to be a grind. I really hope, and we kind of talked about this, I was on a panel or a podcast, a podcast a few months ago with two other students. We talked about renewing this love of learning, and I really think what could help address this potential crisis is recultivating purpose, belonging, and peace in different capacities.
LMB: Amen. Jess.
Jess Deutsch ’91: Thank you. Thank you so much everybody. And it’s always hard to go last.
So I think what I’d like to say is whether or not, and when we first had the conversation together as a group about, and the first question was, is this the title, right? Should we ask the question, is it a crisis or is it obvious that the answer is yes or do we know? And I think all of us can attest to the fact that what we call it is important only in so much as it sort of directs us in what should we do about it, right? And so I think there’s value in considering this as a crisis because a crisis is something we know we want to do something about. And in this case — and I come at this having long ago been a student who was very involved in, I would say nascent conversations about mental health, but we did not have the language for it. So we struggled a lot to even say out loud that we knew that students were struggling.
I had been an RCA, and then there was the conversation in the early, very beginning of the ’90s was, what about students who are no longer in a residential college? Who’s the RA for them? And that was the beginning of recognizing we all need to be in this together and take care of each other. And that was hard to do without a language for it. So it gives me hope that we’re beginning to have a way of talking about this at Reunions, at Princeton. And so some of the issues that we talk about are very particular to Princeton, but they also have versions that exist in the wider world. And so I think that’s instructive too, that this is a place where we have particular versions of mental health crises and we also are human beings.
And so in the work that I did previously at Princeton, which was with students that were heading in a direction of medicine, so students who were very high performing and planning on doing well in the world. And I started to realize there that many of those students while doing very well, their well-being was not in good place. And how important as the future physicians, future caregivers in this country and in the world, it was to pay attention to well-being. And it’s been really gratifying to see that in medical schools across the country now there’s a recognition of physicians need to take care of themselves in order to be able to take care of others. And I think that that’s the model that really inspires me and the work that I do now, which is advising students on next steps in higher education and in graduate school.
And having worked with the student athletes here in the recent past, again, another group of super high-performing students, super high-performing human beings who in many cases underneath the surface were not doing well because they weren’t paying attention to their mental health. And so I think that we are moving forward in acknowledging that, and I hope we get a chance to talk more about what everyone in this room thinks about that question, because the reality is that none of us are in this alone.
And honestly, when Chioma spoke about not having the answer, I think the answer is young people. One of the problems also is this right here, in that students today were born into a world where they were checking here before looking at what’s around them. And I don’t think that this is going away anytime soon, but I just learned from a classmate’s daughter who’s at Stanford — we can talk about other schools right now, right? — there’s a project going on where they’re studying, I think it’s called the lite phone, which is a phone that still lets you text, still lets you call, but doesn’t have social media on it. And it’s not too surprising to find that after using that lite phone for a week, students felt better. So I think there are lots of answers that largely come from young people and hopefully we can continue this conversation all together.
LMB: Thanks, Jess. I want to pivot off of what Chioma said and what you just said about caring for our basic biological needs. I was that student who was at Princeton, the class president of my high school, and I thought that health, when I was in my glory days of my youth, and this was no fault of Princeton’s at all, I owe so much to Princeton University. But I thought health back then was defined as getting good grades, being social, being thin, being active. And then I go to medical school and I think health is about having good cholesterol. It’s about having a normal hemoglobin A1C. It’s about not having the tragic genetic cards dealt to you of the BRCA gene or some other genetic mutation. I thought it was about a set of labs to check. I thought it was about the moment at your annual physical where you get an A plus, and that that was health.
I thought health was about prescribing medications for various illnesses. And I thought health honestly was sometimes about the doctor, like, are we doing enough of a good job counseling our patients? And then you become a patient, as one does when you’re in your middle age, and you become a mother and you see patients for 22 years as I’ve been doing. And you realize that wait a minute, health is actually not an outcome. It’s not a set of boxes to check. It’s not about the moment in your doctor’s office where you get on the scale and you make a little groan. It’s not about getting the news of your new breast cancer diagnosis. It’s not about losing a loved one, it’s about the 364 days a year you’re not in the doctor’s office and it’s about you.
And then I learned that it’s about mental health at the core of each person. It’s about our emotional health. I learned that every patient I’ve seen in the last 22 years has mental health. And guess what, it directly informs the way they think, feel, and behave every single day. So my value add as a doctor is not my degrees and my resume. My value add to my patients is what I have observed for 22 years in human beings and what I’ve observed in myself, which is that health, ergo mental health, is not an outcome. It’s a process. And it’s specifically a process of self-discovery. It’s a process of collecting the facts of our story. Because guess what, when you were bullied on the school bus, when you’re shamed about your weight by your mother, when you had a loved one die when you were young and you experienced some trauma at any age. When you got swept up in social media and felt yourself going down a rabbit hole of anxiety and fear and comparison culture. When you experienced discrimination, when you experienced loss, those all informed your thoughts and your feelings, which then inform your behaviors. The way you relate to alcohol, the way you relate to food, the way you relate to other people, the way you show up at work.
In your relationships with your community and with yourself and the way you care for yourself. The privilege of saying, I deserve to meet my basic biological needs of eating, sleeping, relating to other people. Those are not privileges, those are rights to give ourselves. When you realize that you are entitled to have feelings and you’re entitled to the truth about your story and how it affects your everyday life and your health, but guess what, your blood pressure and your hemoglobin A1C and the weight, the number on the scale, then you’re really redefining health. You’re redefining health as the process of awareness of your facts, awareness of your story, of course awareness of your medical data. You need to know your cholesterol and your hemoglobin A1C and your BRCA gene status if you have a family history of breast cancer. But it’s this process of awareness of your facts, including your story, acceptance of the parts of those facts you cannot control. There are things we can’t control in our life, other people, genetic predispositions toward disease, traumas, the things that happen to us.
And then when you accept those painful truths, and by the way, acceptance is the hardest part of being human. Acceptance as I say to my patients is a bitch. Acceptance is a pain. Accepting the things that we don’t want, that we can’t control. Acceptance is difficult, but when you do the hard work of accepting the parts of your life, your story, your health that you cannot control, then guess what? We have so much more agency than we think. We have a whole ocean of tools available to us to advance our health as conceptualized, as conceived of as a process. It includes social connection, it includes putting down the phone, it includes putting a boundary around people that are not treating you well. It includes advocating for your own health and well-being in the workplace, in your family, with your parents, with your kids. It includes saying that I have feelings too and they matter.
I don’t need to talk about my feelings all day long and make everyone revolve around my feelings every single day of the week, but I’m entitled to feelings. And when we make that known, when we give ourselves permission to be human and permission to acknowledge that the fact that you were bullied on the school bus affects how you eat and stress eat at work, which affects your diabetes, then we’re rocking and rolling. Then we can talk about treating your diabetes and your weight problems, not just with a finger wag from the doctor, but rather a holistic plan to treat your mental and physical health. We can talk about Metformin and insulin and we can talk about addressing the childhood trauma that informs how you relate to food. So what I’m hoping for, and I will end this quickly, is that we can reconceptualize mental health not as an outcome. It’s not about a certain number on the scale or an Ivy League degree. It’s about awareness of our story, our facts, and just being a little more OK tomorrow than you are today with that knowledge.
OK, the next question is, I’m going to start with Jeremy again. We’re going to talk about, oh my gosh, where’s the next question. The next question is what is the most important area to pay attention to? If you’re thinking about this crisis, lowercase or uppercase C, what is the most important area to focus on, to navigate? If you were to ask this audience to leave with a set of questions to ask themselves, a set of areas to focus on, what would that be?
JN: Is that, you gave a multiple choice?
LMB: So I asked you seven questions in one question.
JN: No, I’m just kidding. You did. I noticed that.
LMB: I know, because there’s no answer.
JN: Right. So first of all, I think we could probably get a sense just from the breadth of things shared by the panel, how broad the definition is of mental health, so and let alone crisis. And so we think, OK, what to focus on. That’s a really great question because it’s a big landscape, and I just want to build on what Dr. McBride said about what you can control and what you can’t control. So if you think about the current crisis right now, however you want to put it, I think we all understand there’s been an acceleration of a kind of uncertainty where we don’t know what’s going to happen next politically, economically, even safety on our streets. So there’s that kind of uncertainty. Then we see just these unbalanced forces, incredible divides between the haves and the have nots, just the disparities of opportunity and so on.
So these are all externalities. Right, so here we are, we’re trying to navigate, our brain’s trying to make sense of all of these things, and our brain really has one major job, which is to make sure we survive. So it’s trying to decide are these threats or opportunities and, how do I navigate it?
But then the other thing Dr. McBride said is that there are resources we could reinforce within ourselves that give us a greater likelihood of being able to navigate all of these challenging externalities effectively. And so what I’ve been really focused on for the last 10 years is trying to understand what is it that gives us a sense of self-confidence, self-efficacy, that we actually can make sense of the world in a way that allows us to navigate it.
And I actually think it has to do with, and the word “loneliness” is very popular. In the title of my book I use “crisis of disconnection” because I think loneliness is often viewed too narrowly by people. In part because there are different types of loneliness, and by the way, we’ve touched on all of it here. So one way I think about loneliness is there are three types. First is what most people think of, where’s my friend? Where’s someone I could tell my troubles to? A confidant. Who doesn’t imagine life could be easier if you had someone you could share some of the challenges with, and that’s true. But as we started doing the research and doing programs, including we’re now active on 35 campuses and looking at ways to connect people, another type of loneliness is systematic exclusion, right? So that’s because of race, of gender, of disability, of income. So that’s different than not having a friend. You’re being systematically discriminated against or excluded or disadvantaged because of some characteristic. So call that societal loneliness.
The third type, which I actually think, and we’ve touched on this, may be the most problematic and call it spiritual or existential. As I’m navigating the world, who the heck am I? Who am I? And does my life have meaning and purpose and consequence? Does my life matter? And if you don’t have a sense of positivity around that, it becomes very, very difficult to imagine how you’re going to navigate all these challenges and complexities. So this may be over-simplistic, but obviously sometimes simplifying things, at least lets you get started. I have an increasing sense that if we could figure out a way to be better connected to ourselves — and there are variety of ways we could do that — to the people around us, friends, neighbors, even community, and here’s the big one, to the bigger human story of what we’re navigating in the biggest sense that gives our life meaning, purpose, consequence, then mental health is no longer a crisis. As Dr. McBride says, it’s something we explore. It’s living.
And I’m very optimistic, now we could begin to frame our understanding to do that. Why? Because in the work we’ve been doing through Project Unlonely, we see people responding. Not just on campus, older adults in community activities. So there’s something people respond to when you say, you need the skills, the resources, the sense of possibility to navigate the challenge, because you’re not going to avoid challenge. Whether it’s getting the BRCA gene, or a terrible gene, or other kinds of external effects — those are going to be out there. The question is how do we navigate them? And then the question as an educator is, can I be part of a system that invites our students as well as our faculty and staff to develop the capabilities to most successfully navigate the challenges towards what you might call health or an integrated way of navigating the world with a sense of comfort, ease, safety, and satisfaction.
LMB: Joshua?
JB: Big shoes to fill there. Well, I’m a child psychiatrist by training, and so I’m going to answer this in sort of two parts. One is family based, and the other idea is personal. When I was trying to conceptualize how to sum this up, I mean it’s such a big topic and you wonder, how do I make sense of this? And it’s very easy, I think with very big topics, to become overwhelmed and not know where to start. I talk about this with so many of my patients because they’ll be like, “oh, I have this final paper, or I have a thesis or whatever to do, and I haven’t started yet. I don’t know where to start. I think about all the things I have to do and I don’t do anything. I can’t focus on, distill it down to one thing.” So I’m going to try, if possible, I don’t know how successful I’ll be, but to try to distill a couple of these ideas into some things that each and every one of you can take away from this and hopefully start doing.
Because I think when we look at, even though we’re talking about student mental health, we’re talking about what’s happening with college students, I really think this is a broader issue affecting many other demographics beyond this. So sometimes these discussions become generational versus generational, and maybe it’s the job of the older generation to gaslight the new one. Maybe children inevitably pay for the sins of their fathers. But arguing about it I think is pointless because I think ultimately there’s a lot that we can do. So what I may say may ruffle some feathers, but I’ll say it anyway.
So here’s a couple things, two songs I’ll refer to. The first song is, have you ever heard the Crosby Stills and Nash song, “Teach Your Children”? Yeah. So you may have some sense of what I’m talking about. I’m going to start first of all with the idea of parents, because ultimately parents are the ones who care the most about the well-being of their children. When a university sends a student home on a medical leave of absence, even if the university has not been able to say anything about that student’s well-being, now it’s the parent’s problem, even if they have no idea what was going on with their student. And I’ve had a number of those conversations with parents after the fact, and many of them say, I wish I had known.
So teach your children. I mean, I think not all of us are parents. Many of us will be in a parental role or caretaking role of some capacity. Do the best you can with what you have. Be a good parent. You don’t have to be perfect. Perfection is not required. It’s good for children and those who you’re taking care of to know that mistakes are only mistakes if you fail to learn from them. So I’ve often thought that if we were able to eliminate a lot of the bad stuff that happens in childhood during the formative years, we probably wouldn’t really have a whole lot of need for mental health services. If you’re able to eliminate trauma of various kinds, physical, verbal, emotional, sexual, neglect, parentification, people know what that word means?
Audience member: Taking on a caregiver role when you’re the one who needs care.
JB: Yeah, this is something I talk about with many, many students because sometimes people will be forced to take on adult roles before they’re ready. So if they’re dealing with, let’s say, I don’t know, a parent who has a history of alcohol issues, so now the student is taking care of them in various ways or covering for them or doing things that they normally would do but can’t for whatever reason. And so we often look at those people as children and say, “oh, you’re so precocious, you’re so adult-like.” But yet at the same time, those are the same people that at some point, 20, 30, whatever years later, realize, “I didn’t have a childhood.” So in my case those are the students that I end up seeing who realize it a little bit earlier.
But none of that’s free. So your body, as I often tell folks, we have a set response to traumatic things. It doesn’t matter if it’s physical, verbal, emotional, whatever, our body goes through a whole cascade of things that happen to us to protect us. But when those stresses become chronic as opposed to acute things, our body doesn’t really know the difference. It just continues to ring the alarm bells. And so teach your children.
The other thing is another song. I’m going to paraphrase a lyricist, Siedah Garrett, who wrote the song “Man In the Mirror.” So what she said, “If you want to make the world a better place, look at yourself and make a change.” Later sung by Michael Jackson. So what does that really mean? How do we do that? I mean, there’s so many ways that we’ve already touched on a couple of them. I tried to distill them down to a couple things that I try to talk about with my own patients and try to mirror in my own life. So if you ever read the book, The Book of Five Rings, five elements, earth, water, wind, fire, and the void. So going to touch on all those things. And these are all things that I think every single person in this room, every single one of us can do in some capacity.
So earth is grounded. So find things in your life that help you find your center, get grounded, and on a very practical level, get outside. Human beings were not meant to sit at a desk in front of a computer, get outside. Two, water. Water is fluid. Water finds the lowest point. Teaching people how to resolve conflict or mirroring that is a skill. We cannot rely on leaders and governments to do this because they fail time and time again to do that. So if we can do that in some way, in some capacity, and show people how to do that, that’s often helpful. And because the less black and white, positive and negative, we tend to see the world, the more room there is for gray. The more room there is for nuance. It’s one of those things, unfortunately, social media does not do very well.
Fire. Fire is passion. Finding things that you enjoy and are passionate about. My wife, who’s in the audience managing our children, we often have this conversation about the middle-age doldrums. As you’re grinding through life, doing all the things you need to do to get through the day, to go to show up for work and take care of your kids and pack the lunches and take out the garbage and all this stuff. In the process of doing all those things, yes, those things have to be done, but there’s a part of you that often gets lost as well. Reference another movie, 1985, Breakfast Club, if you guys remember the Ally Sheedy character who said, “When you grow up, your heart dies.” It doesn’t have to be that way. You don’t necessarily have to let those parts of yourself die, but you do have to keep them alive. And you do have to stoke those embers every now and then. And it’s very helpful for folks that you are children and everybody that you are in your life to see that it’s possible to do those things. It gives them hope to do those things too.
Wind. Wind is movement. Move. I spend a countless amount of time trying to get my patients to move more. This probably applies less or so to the athletes, but even so during finals time, midterms, everybody’s body hurts because they’re spending so much time sitting in a chair. And with that whole stress response, one of the things that happens is our bodies tighten up. It’s a protected response. Tighten up midline structures to protect your neck, your internal organs and so forth. And that leads to a lot of pain. And so moving, getting the blood flow going is important. We don’t necessarily need to move a lot, but something is better than nothing.
This is a study that I’ll sometimes reference with my patients, and you can find it, you can look it up. It’s a number of years old at this point. It’s about exercise and the minimum duration needed to affect some kind of mental health change. They were specifically looking at what they call green exercise or exercise done outdoors, but they’re looking at a whole bunch of things, even things like gardening and camping and stuff like that, you wouldn’t necessarily consider traditional working out. Does anybody want to take a guess how long, what was the biggest bang for your buck? How long someone needed to exercise?
Audience member: 25 minutes.
JB: 25 minutes. Go a little-
Audience member: Five, it’s five.
JB: Yeah, five minutes. Five minutes. We can all find five minutes. There was another study that was done with college students, having them ride an exercise bike, and about 60% of their VO2 max, what we sometimes call zone two training, so they can carry on a conversation. And the answer there was 10 minutes. So it doesn’t necessarily require a lot, but getting up and moving.
And the last thing is void. That’s the translation that often gets used, but void really means possibility, creativity. Find things that you can do that give you a sense that you’re creating something and discovering something. When we go from discovery, when we’re trying to discover things, we’re in less defensive mode. And so all the things that children naturally do, they play with clay, they draw, they do these things that are artistic, there’s no necessarily reason why we have to not do those as adults, but we often get told in various ways that those are things for children to do.
So I think in various ways, these are things that every single one of us can do in some capacity. I don’t actually think it is fair for us as people to put this on the shoulders of young people. So this is your crisis, you deal with it, because they didn’t put themselves in it. Older generations are the ones that created the technologies that are implicated in some of these things. So in various ways, we all have, I think, a responsibility to do whatever we can individually to make aspects of this better. Because when we take care of ourselves, the people around us get taken care of too.
LMB: Chioma.
CU: Thank you, Dr. Blum. That was beautiful. Especially the five elements, like practical takeaways from this talk. I’d like to go back to the subject of externalities and societal loneliness and paint a couple of pictures for you all.
Imagine waking up next to a landfill. It’s an ugly sight. It smells. It somehow affects your getting out of the day, getting up out of the bed, starting your day. But you have to go to work regardless. You work at a local factory, you have to get the kids ready for school. The dryer is not working, so you hang your clothes out. They also have a stench, they might be a little blackened from the nearby train that comes through your neighborhood to drop off trash at the landfill or ship cargo throughout the neighborhood or somewhere else. Those are images, smells, sounds of people’s lived realities. And they affect not just physical health, but mental health, emotional health, spiritual health. Health well-being is holistic and it’s also structural.
Most people, I dare to say in the world, face some sort of systemic injustice, and they just have to deal with that, unfortunately. Whether it’s because of their gender identity or their disability status or their race, their income, even their religious practice. Most people in the world face these daily struggles and often overlapping struggles holding multiple marginalized identities. And so I would say when we’re talking about mental health, when we’re talking about health and well-being, generally, they’re inseparable from social justice.
And these systems of inequality are ones that we’re all complicit in to some extent, and they’re bigger than any one person, but I dare say that there is something that each of us can do to minimize harm at the very least in what we do and just who we are to each other. And it can be really small actions of actually acknowledging the person that y’all are sitting next to on the bus, on the way to work, or buying the groceries for someone in front of you if you’re stopping by getting groceries in a lower income area.
And not making a huge scene about it, but just paying it forward in some way because you never know what that person’s dealing with. And even if they are struggling to find money to take public transportation, to go to the doctor’s office for their appointment or to pick up their kids or to get groceries, and you help out in that kind of way, that can minimize stress. And that stress, as we talked about and will probably continue to, builds up in the body and even minimizing it, maybe minimally can have a sort of ripple effect that no one can even quantify or will ever be recorded in any book, but is meaningful nonetheless.
So yeah, when we’re talking about well-being, I just wanted to throw that out there. It’s no practical takeaways, but just thinking broadly, how can we each not just talk about but embody health and well-being for ourselves and for other people.
LMB: Jess.
JD: Thank you. Yeah, when I thought about what do I focus on or what do I think we can focus on, I think about when I’m meeting with students in distress. A couple of simple things come to mind that have been effective and that I’ve continued to think about. One of them is to ask the question, how are you? And really wait for the answer, really wait sometimes because the kind of reflective answer, especially around here, is “I’m good, I’m good.” And then when you just sit with that a little bit, the more complicated story can come out. And I think really being willing to ask a question and listen, look for it and listen to real answers allows us to have more honest conversations about how we’re all doing. And so asking that question genuinely is different from the casual throwaway version of it that I think is kind of like the MO of our culture. So that’s one simple thing.
I also think a lot about when I was doing the health professions advising work, a student came to me one day very sincerely to show me his calendar and to show me that he had a space in the calendar on, I think it was Tuesday, from 4 to 4:20. There was nothing there, and everything else was very, very filled out and busy. And he wanted to know if he’s going to be a good applicant to medical school next year, what should he put in that space? And he really wanted me to give him an answer. Like there was a right answer, and I had it. And I asked him, I thought about it for a second, and I asked, have you ever walked on the towpath? And he looked at me like I was completely crazy and I really meant it. And I think a lot of students graduate from Princeton never walk on the towpath. But the idea of getting grounded in nature, in just taking a moment for yourself, it really is a part of being able to perform at your highest level and being well. And so again, reminder to pay attention to the world around you and to take those kinds of breaks I think is really a part of something that we can do.
And the third thing, which maybe we can do a little exercise of it in here, because no matter how many times I do this or what different context in which I do it, I always kind of notice the impact. And that’s just to take a deep breath. And my daughter is looking at me because she knew I was going to say that. I say it in our home, I say it in my work, I say it to myself. So can we all just take a deep breath?
LMB: Thank you. Thanks for this.
JD: Right. I think I notice it makes a difference, and it is a simple thing that you always, no matter what is going on, no matter what level of crisis, the opportunity to take a deep breath is something that we carry with us.
LMB: Thanks, Jess. I’m going to make my closing remarks really brief because we want to open it up to questions. Joshua, you stole my thunder because I love what you said about, I mean, you’re talking about meeting your basic biological needs to the extent that that is possible. Feeding your body, moving your body, resting your body, and giving yourself space for creativity, meaning, and purpose. And at the core of it, we all have access to that within ourselves. We may not have access to nourishing foods. We may not have access to fancy gyms or Lululemon leggings. Those are not necessary. As I say to patients all the time, exercise doesn’t need to be formal, fanatical, or fancy, the three F’s, it just needs to happen. It can be five minutes.
Nourishing your body doesn’t need to be with a fancy meal, it just needs to be food. One of the best ways to quell anxiety and to build attention, focus and optimize your cognitive health is not by getting supplements from the wellness industry necessarily, it’s about eating lunch. So if I had one tip for so many of my patients, what’s the best diet out there? The diet that’s the best out there for you is the diet that nourishes your body and nourishes your mind on a regular cadence. Eat lunch if you’re able to, if you can have protein, fiber, and healthy fats, that’s great. And then it’s about resting your body. Resting your brain. I used to think rest was a luxury. I used to think mental health was a luxury item. Guess what, those are not luxury items. Those are essential, basic biological needs — to get rest, to get sleep. And if you’re not getting rest or sleep, let’s figure out who to ask for help.
And then the final thing I want to close on is about truth and trust. So we live in a world where the American medical system is failing people, is treating patients like boxes to check and cattle to herd. And if you’re lucky enough to be able to afford it, you can have a doctor who pays attention to you more than for five minutes through no fault of the doctors who are in the system. And that has birthed the wellness industry. The wellness industry is a multi-multi-billion dollar industry that is thriving because our medical industrial complex is failing people. So people go to the doctor, they get their labs checked, they don’t feel well, they go on the internet. I understand it. I do it too. I love Dr. Google. I love little gizmos and gadgets. I have some in my own house. I pop vitamins just because it makes me feel better. Placebo effect is a wonderful thing. There’s also evidence to show that people with iron deficiency need iron.
What I’m saying is be careful who you trust. And it’s not to say don’t trust anyone, as saying to recognize that every messenger has bias. I have bias. The wellness industry has bias. Make sure that you are getting trusted fact-based information about health, body, and mind. Because even some of the most, well-intended physical health practitioners, nutritionists, exercise physiologists have bias. We all do. That’s part of the human condition. But just be careful and make sure that at least the guides that I trust from my own health and well-being and in my regular life are people who have humility about what they don’t know, who acknowledge when they make a mistake and who engage in a collaborative process. And they don’t claim that they have moral high ground over the person they’re counseling.
I’m going to end there and just say thank you guys so much. Thank you to the panelists for being such just wonderful messengers and humble ambassadors of the message of mental health mattering. And let’s open it up for questions.
Audience member: Yes, I’m interested in stuff that Princeton might do as an institution to be helpful. Specific actions. I mean, I’m thinking of things like if we said we’re going to take a little caseload or workload off so everybody can spend 20 minutes on a towpath every day. Or with regard to the anxiety about jobs after Princeton, if we would use career counseling to show people, if you don’t make it into medical school, you don’t get into Goldman Sachs, you still might have a life ahead of yourself. It seems to me that these are things that possibly the University could do that would be specific to help these kind of generalized problems that we all know we’ve got. You guys must have a lot more thoughts than I, and those two things popped out of my mind, and they’re probably wrong, but...
LMB: Who wants to take that?
CU: I could start briefly, so like it says in the handout, I’ve been a part of many mental health task force committees addressing this very issue. Princeton is even working with the Jed Foundation currently, which is this suicide prevention organization, to again, address this. And I would say from countless meetings with the CPUC, the Princeton Council and student meetings, this idea of academic rigor is very hard to sort of shake here at Princeton. And one of my colleagues just walked in who is very familiar with this. You all should go to his talk at 4 p.m., we’ll talk about that later. Academic rigor. And of course, many of us in here were Princeton alums, soon to be, and we know that’s kind of part of the culture. But it feels like we’ve outgrown prioritizing academic rigor over all other values at this university. Why can’t we hold health and well-being at the same esteem and the same regard as academic rigor or excellence?
Right now, it seems as though from the student perspective, administrators and staff are working tirelessly to correct this. But it just seems time and again, that we’re valuing students’ grades, turning things in at a particular time, these long, thoughtful, really critical essays that do sharpen our skills. We’re valuing these much more than we’re valuing sleeping, getting lunch, taking a walk outside, et cetera. And when your professor tells you you need to meet these deadlines and there are no exceptions, not even if they can drop the lowest homework grade even, or grant an extension, you seem to feel like you have to meet those expectations or else you will be punished. In other words, you might be punished or penalized for evaluating, taking care of your mental emotional well-being.
So in short, from my perspective, I really think we can reevaluate the standards of academic excellence at this university. And I’m not saying everything is pass fail, but I’m saying institutionally make it such that professors, all professors have to drop the lowest homework grade. Or the exam that you did the best on is weighted a little bit higher, more, than the other exams that you took in that particular class. So you’re still challenging the student, but you’re also giving them leeway to make mistakes and take care of their well-being in the ways that they see fit.
JD: I also just want to add that, this is a good place to do a commercial for the session that’s happening at four o’clock. McCosh 46, right, Zhan? And the focus will be specifically actions and activity on this campus related to this issue. And I encourage you all to attend that four o’clock session.
LMB: Let’s wait for the microphone, Peter, is there a microphone going around to ask the next question?
JB: While you’re doing that, just one thing to throw to your question. I can’t speak to Princeton, I don’t work here. But one thing I would like to see kind of across the board in universities is a step-up in mentorship because I think that a lot of the questions that people have, have been repeated time and time again. It’s very helpful, I mean I think maybe Princeton probably does more with that in terms of the alumni network. But I would like to see that, particularly a lot of students who are struggling, with a university may know ahead of time may struggle, I would like to see more attention placed with those students because it’s not like when you get here, oh, then you’re good. You figure it out. It means you’re going to need ongoing attention.
Audience member: So I’m a child psychiatrist. I work for NYU Medical Center. I work in a Hackensack, New Jersey, office. So just broadly, challenges that I have as a psychiatrist. I work in New Jersey. My licenses are in New York and New Jersey. My student goes to Susquehanna, Penn State, I cannot see them. They go off. I say, we’re just going to hope you do well, we’re going to bring you back in October, November. Sometimes it is too late, OK? Then maybe they’re struggling. Maybe the university knew they were struggling, maybe they had mental health problems before they went. But we have FERPA, right? FERPA, which is, it’s a federal, it’s a protection that parents are not allowed to know both the academic and the health information for their students unless the student specifically waives it. So your student isn’t doing well, you’re not told, and maybe emails that assignments aren’t getting done, that goes to the student, not to the parents. And then very quickly as the outpatient psychiatrist, I’m told, ooh, so-and-so is advised by their adviser to take the semester off. And by the way, doctor, can you please write a medical note justifying what we’ve already done so now we can get our money back from the university or from the insurance.
But it’s like when it goes bad for the students, it goes bad so quickly. And I’ll say before any patient goes off to college, I say, let’s look at the help, let’s go on the website, let’s look at the building. Does this look familiar? Let’s go over how you can get services. And just time and time again I’m hearing, I couldn’t get in. There were no appointments. I went, they weren’t good. I’m like, please give them my number. No one calls me. And this is just the story. Again, some kids go off to college and they do really well. They come see me on the vacations and it works out beautifully. And then when it goes bad, it goes back so quickly we cannot stop it. And parents are in the dark. And universities, I think between, to be honest, hide behind FERPA in some ways and then it goes bad and there’s nothing that parents or anyone can do until it’s too late.
LMB: I feel you. I think it’s not hyperbole to say, I think it’s really a moral crime. The children and adolescents in college are not allowed to have access to their psychiatrists or their therapists across state lines. That is a moral crime. You’re in the relationship business, you’re in the relationship, the trust that you have built with your patients, the trust that you have built, it’s not sufficient for their health, but it is necessary for their health. To have to redo that is awful. I also would say, but I don’t want to land on doom and gloom, I would also say that you’re talking about just the American health-care system in general, which I think we all can agree is broken at best.
I think one of the solutions, which is not a total solution, is to acknowledge the harms of the pandemic. It was a parallel pandemic of mental health and crisis and it’s only just beginning to play out. And I think that the service you can do is somewhat like what Josh was saying. That is to as parents acknowledge before your child goes off to college, acknowledge that regardless of your socioeconomic status, your race, your gender identity, or what kind of school you came from, whether it’s Princeton or somewhere else, acknowledge the toll of loneliness, social isolation, social media, comparison culture, the world as it is. Acknowledge that, and let’s talk honestly with our students about where are you on the continuum of mental health when it comes to anxiety. Because guess what, you have anxiety. It’s not a question of do you have anxiety, we all do. If you didn’t, you wouldn’t turn in your term papers. Where are you on the continuum and what tools do you have to bring with you to college to pull the anxiety back from a 15 to an 8.
Where are you in the continuum of depression and mood? Because we all get depressed, little “d” depressed. We all get excited when we get asked on a date. Where are you on the continuum at baseline and what tools do you have to bring yourself out of a funk. Who are you going to call? Who are you going to ask? What do you need? And then have a low threshold for asking for help before you go to college and then prayer that your kid does OK, because they have suffered uniquely because of the pandemic in myriad different ways, as diverse as the stars in the sky. But I think we have to have that conversation as parents before they go to college. I know I am with my three kids, one of whom’s going to be here in the fall, and even though she’s the kid who looks like she’s got it all together on paper, we are going to have that conversation, we already are, about let’s stop and talk about how are you coping? It doesn’t have to be with me, but let’s talk about it. Who are your people? Who are your trusted allies? Because I think it’s a crime that kids aren’t given access and we are to blame as adults for the system.
JB: I can speak from the other perspective. So I’m usually in the perspective of, I’m the psychiatrist trying to reach the child or adult psychiatrist back home or the primary care doctor, and I have equally difficult time often getting in touch with them because we’re all busy, we’re all seeing patients, playing phone tag and stuff like that. I can certainly tell you what I do with my patients who are going off to graduate school because we do the exact same things, same exact struggle, and I just did this with so many folks in the last couple weeks. We do the exact same thing that you’re probably doing, we go on the website. In some cases we’ll sign a release that says, gives us permission to send records, and sometimes I’ll send a note or whatever ahead of time. I would say it doesn’t always work. In fact, probably it’s more the exception than the rule that it actually works, even though I know ahead of time that this would make things easier and the students will often acknowledge that, yes, yes, please do this.
I once sent some records to a university, someone was going to be going to via fax and they sent the fax back and says, we don’t need these yet. I was like, do you not understand how fax works? It didn’t make any sense, but that’s often where we’re at. It’s just so ridiculous. I mean, I think the difficulty is in communicating and I think people hide behind HIPAA and all this other stuff, blah, blah, blah, blah. But I mean I think a lot of those things often get in the way.
I think the thing that I try to do, and again, I don’t know how successful I do this, and I’ve seen this. I remember once trying to refer a patient to see an ophthalmologist because of some issues he was having that may have been connected with the dose of the medication we were using. Either way, the office was not able to get in touch with him because his voicemail was full and he wouldn’t answer the phone. I was like, well, can you send him a letter? Can you send him an email? They’re like, we can’t do that. So I’m often trying to physically make the phone call with them because I know that if they encounter a barrier with our incredibly easy and whatever, smooth sailing medical system, I mean I’m sure many of you who’ve been a patient in our medical system, how complicated and convoluted it is to deal with insurance and find appointments.
If I try to refer people back to my own hospital that I’m contracted by, their first available is October. So when folks encounter those kind of barriers, they’re like, I’m not going to put up with this, but they’re often stuck about what to do next. So I think we go through, try to do through, OK, this is plan A, this is plan B, and if it doesn’t work, plan C is often, well call me even if you’ve already graduated and I’ll try to help navigate these things because it’s not unusual a year or two or three afterwards when someone’s finally getting around and making that referral appointment, they’re like, I know I haven’t seen you for two years, can you send those records now?
LMB: Yeah. Catherine. OK.
Audience member: Thank you so much each of you for doing this panel. It’s such an important topic and I’m deeply appreciative. I’m a physician and a mom with zero expertise in mental health, so I really have no idea what the solutions are, but something Chioma said really hit me, which was how your generation has been bombarded with education about mental health for so many years and so many years, and yet we’re still doing so badly. And I loved how Dr. McBride, that you call it mental health, not mental illness.
But I wanted to hear your expert comments. I’m sure you all have seen Abigail Shrier’s book that’s gotten so much press recently and I have no idea if she’s right or not, but I thought she made a really compelling argument that maybe we’ve been spending too much time focused on social-emotional learning from a very young age and kids are learned from a very young age to think only about themselves and every little feeling and then they pathologize normal experiences, if I’m probably paraphrasing her incorrectly. But I would love to hear your expert thoughts on this ongoing debate.
LMB: I would love to take that if I can, not just because I know you, Catherine. I think there is an argument to be made that, like in Abigail Shrier’s book for example, she makes the argument that I think that the title of the book is Bad Therapy or something like that.
I think that there’s an argument to be made that therapy, psychotherapy for example, can sometimes do more harm than good for an individual. For example, my patient who’s been in therapy for 20 years but is still in an abusive relationship and unfortunately that relationship and therapy has accidentally inadvertently enabled this person from actually leaving at the expense of their safety. Now, that’s not to blame any, there are also patients I have who are in therapy trying to figure out their interior landscape and just need to go to AA and quit drinking. So I think, I mean as if that was easy. Or people who need to be on medication in conjunction with psychotherapy.
So I’m answering your question in a little bit of a roundabout way, which is to say that I think that the way we address mental health is nuanced depending on the person. So for some people it’s Prozac, for some people it’s therapy. For some people it’s climbing mountains. For some people it’s finding meaning and purpose. For some people it’s acknowledging their childhood trauma, acknowledging the discrimination they face in their life and then giving themselves permission to be seen and heard in their community. And for some people it’s a combination of all of those things. So when you ask the question, are we mentally masturbating about mental health at the expense of thinking about broader issues like climate change and social justice, and I think that we do run the risk of thinking about ourselves. I think there’s a fine line between self-awareness and self-indulgence. I actually do.
I also think that to the extent that we all own mental health, we all have mental health and that our mental health is expressed whether we like it or not, to our bodies and to our communities, that we ought to know about our mental health and query our own interior landscape to know how we’re affecting other people. To know how we are inadvertently enabling systems and families and communities because that is mental health too. There’s no kind of mental health and mental illness. You’re either on one side or the other. It’s not like tastes great, less filling. We’re all on this journey.
So my point is that yes, it’s possible to overindulge in psychotherapy or in the mental musings of my own mental health. But I think the point that’s happening now, and it’s a beautiful thing in our culture, is that we are acknowledging that mental health is universal. That there’s no human being without mental health, and let’s name it and let’s work on it when our mental health is on the fritz. And if your mental health is dandy, then go do good with it and help someone else.
JB: I guess one thing I’ll also say about that is that if you look at a lot of the world’s religions and philosophies and so forth, they don’t often talk about, spend more time thinking about yourself.
LMB: That’s a great point.
JB: Charity to others and often if you ask people what makes you happy, pursuing happiness in itself is sort of a fool’s [errand], right? Because you chase it, but what do you find is sort of ephemeral. If you’ve ever been a kid and you get a couple bucks for your allowance and you blow it on chips and bubble gum and you’re like, oh, where did my money go? And I think when we think about broader things, things that people can find that they get out of themselves, and if nothing else, even if they’re not necessarily out of themselves, at least get moving, go on to the next thing. Things will, a body at rest stays at rest and vice versa. I think the focus on yourself and probably some of the impact of social media and so forth, which is by definition branding yourself, it’s like a microscope, right? Everything, when you see it, it looks really, really big and then you can’t see the bigger picture.
JN: I just want to grab this, kind of build on exactly what Josh said because, and just his pointing us towards thousands of years of cultural expertise manifested by some pretty successful religions. Not saying to think more about your own inner crisis and turmoil, although there’s plenty of that in religion too. And to anticipate a final moment in panels like this, when people say, is there just one piece of advice? So I think it actually builds on what y’all said, to actually become part of a bigger story than your own concerns. And there are three very straightforward ways to do it.
OK. So one is really get out in nature and pay attention to how amazing it is, even when it’s raining and access awe and wonder and all the feelings of that, including the psychobiology of awe and wonder, which is amazing and increases compassion, empathy, reduces blood pressure and so on. And so, nature.
The second is serve other people. Nothing introduces you to the bigger story of human misery than finding someone you can help and help them. And the third is actually to access creativity and imagination to pay more attention to the world and to see it in a different way, and particularly the wonder and the awe and so on, again, within which your story, as precious as it is to you, actually becomes smaller in your own estimation of it. And I think these are the kind of things that can be promoted at Princeton and other places really as guidance, not rules, but guidance. And I think that allows us to still cherish and pursue our personal story both within a bigger context.
LMB One more question or two more? We’ll, we’ve got a few. Oh yes, go for it.
Audience member: Yeah, thanks. Great panel, can people hear me? My name’s Cam Stout, Class of 1980. And I think the one thing we need to tap into is the lived experience of alums. I share mine. I’m an alcoholic. I went through a huge depression, capital D in depression in 2013. I’m a successful lawyer, but I spend a lot of time sharing my story. And there is zero shame in that and I would love to see more alums, this isn’t judgey or preachy, but I think it’s important for us to share with students. So I do mentoring of first-generation low-income students here. I live a mile down the road and I share all the time. And it builds a community that we all live in together. And so my question I guess is, and Jess, you alluded to this in your PAWcast with Calvin Chin, what can alums do to make this happen more and to share, and find the courage to share. And believe me folks, it takes me no courage to share anymore. I think it’s important to doing it. So thank you.
JD: Thank you. I’ll just jump in here to say that I think it’s exactly what you just said, it’s sharing stories and making those stories a part of the experience of what it means to be a part of the Princeton community. And so being here and making these stories a part of the experience of being at Reunions and being on campus, being in the progression of student exposure experience while they’re on campus, I think that that’s what I would say is the answer. And having written The Whole Student column for the last couple of months, I would say each time a new column comes out, someone shares their story. And so we’re kind of figuring out in the magazine what’s the way that we can continue to do that. And I think that there are students really hungry to hear those stories and to be in conversation and recognize that there’s no one trajectory and that we learn a lot from each other. So thank you for sharing yours, and hopefully we continue to build the opportunities to have that happen.
LMB: Yes.
Audience member: Real quickly, Zhan Okuda-Lim, Class of 2015, I want to thank all of you and the PAW for organizing this panel. As Jess mentioned, I’ll be moderating a companion panel at four o’clock in McCosh 46 with some current students and also administrators from the Office for Campus Life to talk about specific challenges and opportunities for Princeton around mental health. If you’ll excuse me, I need to go set up for that panel, but I hope a little bit later this afternoon you’ll all take our advice around being out in nature, getting the blood flowing, and can join us at 4 p.m. in McCosh 46. And I think there’s another question here, so I’ll hand the mic over. Thank you.
Audience member: Do we have time for one more?
LMB: Yes, we do.
Audience member: And maybe not the best question to end with, but since we are Reunions and we have lots of different generations, I guess my question is more about my generation, older, is what capacity for change in mental health do you see in older Americans and does it get bigger or smaller as they get older?
LMB: I mean, I can speak really quickly, really brief, just as a primary care doctor seeing patients all ages. My oldest patient is 96. I think there’s a false assumption that with age comes more depression, more loneliness, and it’s just not an inevitability. And I’m not saying that because I’m an optimist, which I am. I’m saying that because with age also comes wisdom and perspective and jettisoning a lot of the expectations about what is health. And also I think that if people experience depression symptoms when they’re older, they have depression, they don’t have “I’m old,” they have depression. I think we under address depression in older Americans. I think we assume people are depressed. Well, of course she’s depressed because her best friend died and she’s widowed. And so I would just say that there’s more agency for anyone talking about mental health than they often think. But maybe that doesn’t answer your question.
Audience member: Well, my usual mantra to myself is, especially as I get older, is you can’t change the habits of a lifetime, which is very comforting in its own way as an excuse. I’m curious as to what capacity there is to change the habits of a lifetime.
LMB: I think there’s always capacity. I think as long as you’re alive, as long as you have today, there’s capacity. I mean, I truly believe in the mantras of AA, even though I’m not a participant in AA myself. The concept of the serenity prayer, which is work on accepting the parts that you can’t control and the agency that you have and then know the difference. I’m totally mangling the serenity prayer by the way. But what I’m saying is that I think we have more control than we do, and it’s also the one day at a time mentality of “we just have today.” And so practicing gratitude, practicing the wisdom of perspective of choices we made that we aren’t proud of. We all have unproud behaviors. We all do things every day that sabotage our health. Forgiveness of oneself is part of growth and part of health.
JB: I think one thing, just to piggyback off that is that if you informally ask people different demographics age-wise, who’s happiest, I think the answer is usually people who are 60 and above. You’re through the grinding years of those middle-age doldrums, you’re kind of at a place where you’re more comfortable hopefully with yourself and the different pluses and minuses. I mean age obviously catches up to all of us, right. We’re talking about trauma, all that cascade of stress-response-type things puts us more at risk for other chronic health issues.
So I think with that in mind though, I mean, I think I’m more optimistic than not. And so I think that this sort of sad thing societally, I mean, I think we often shuttle people after a certain point, after retirement, for example, it is saying we kind forget about them, which I don’t think has to be true.
I don’t know if you ever took a psychology class or anything. There’s a guy, Eric Erickson, he’s a psychoanalyst early 20th century, and he had these different developmental stages that people had to go through to advance to the next stage. And for folks who are older, there was this stage called generativity versus stagnation. You stay the same or you invest in something bigger than yourself, the idea of giving back. And so the people who are maybe in retirement or whatever, who tend to be the happiest are ones who were involved with their communities, involved in other people. Were involved in themselves, they’re trying to make themselves better, have a new career, whatever it is. I think those are the folks that tend to do best mental-health-wise.
LMB: Thank you all for joining us, and I hope you have a wonderful rest of your Reunions Weekend.
PAWcast is a monthly interview podcast produced by the Princeton Alumni Weekly. If you enjoyed this episode, please subscribe. You can find us on Apple Podcasts, Google Podcasts, Spotify, and SoundCloud. You can read transcripts of every episode on our website, paw.princeton.edu. Music for this podcast is licensed from Universal Production Music.
Paw in print
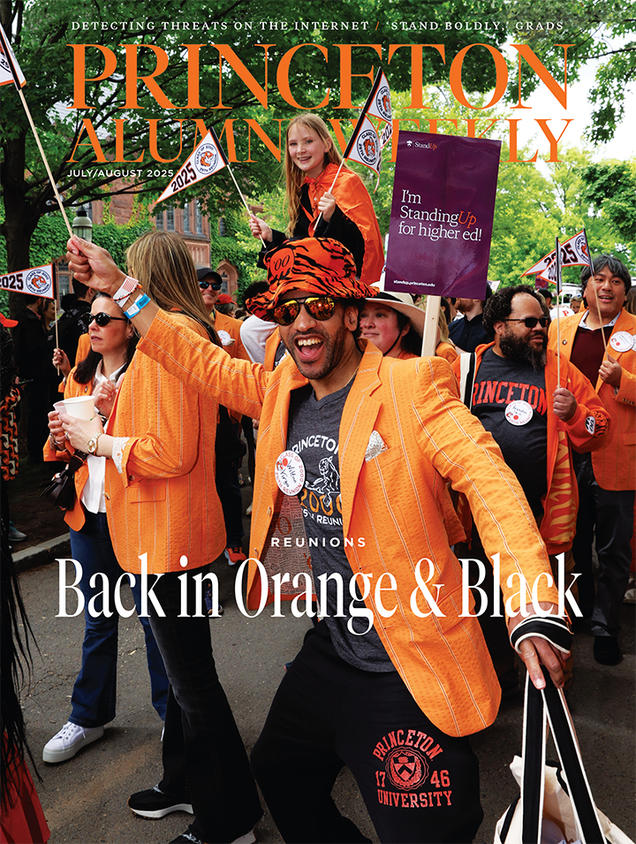
July 2025
On the cover: Wilton Virgo ’00 and his classmates celebrate during the P-rade.


0 Responses