
The Doctor Is On
Céline Gounder ’97, an infectious-disease specialist, moved into the spotlight during COVID — and remains there
It was the 2019 holiday season, and Céline Gounder ’97 didn’t like what she was hearing about a new virus causing pneumonia in a few dozen people in China. When Gounder, an infectious-disease physician, made rounds with medical residents at NYC Health + Hospitals/Bellevue in New York City and told them they soon would likely see patients with the disease, “they were rolling their eyes,” she recalls. But to Gounder, a respiratory virus that was being transmitted within communities, not just within hospitals, suggested it was more infectious than the virus that caused the SARS outbreak in 2003. And the fact that the Chinese government was responding so aggressively signaled the problem was serious — probably more so than the reported patient numbers indicated. “I told them, ‘No, no, this is actually going to be a big deal,’” Gounder remembers in an interview with PAW. She likens that time to being in a burning building and telling everyone to clear out, “and they just sat there … looking at you like you were crazy.”
Gounder bought masks in January 2020, and, thinking ahead to a potential lockdown, a home rowing machine a month later. For the past several years, she’d been bringing her perspective on health to the public by appearing on television and writing for print, alongside her clinical practice. On Feb. 27, she released the first episode of Epidemic, a podcast chronicling what she was already calling a pandemic, even if the World Health Organization wouldn’t officially do so for another two weeks. In that inaugural episode, Gounder and her early co-host, Obama administration Ebola czar Ron Klain, flagged issues that went on to become defining limitations of the early U.S. response to the virus, including conflicting messaging from the government, constrained testing capacity, and underprepared hospitals.
Days later, the first laboratory-confirmed case of COVID was diagnosed in New York City. Over the following three months, the city counted more than 200,000 lab-confirmed cases and over 18,600 deaths from the disease, according to a report from the Centers for Disease Control and Prevention. Bellevue was flooded with critically ill patients, and Gounder found herself working 100-hour weeks between her hospital duties and media appearances. At the peak, she was doing as many as 20 interviews per day, including up to 10 TV appearances. She became one of the pandemic’s most prominent public physicians, which is what physician and writer Bryan Vartabedian calls doctors who consider public engagement as part of their work. The pandemic, like no other health crisis, has put the spotlight on these physicians due to the rapid pace of change in the virus and public health conditions, flood of data and research in need of interpretation, and demand for information to supplement official government communications.
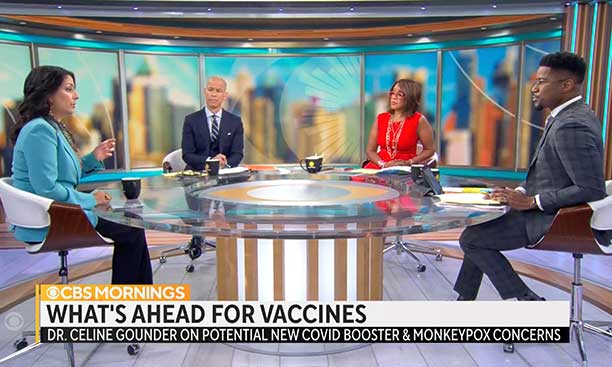
Starting this year, Gounder turned most of her focus to journalism. She will still be spending four weeks per year on the Bellevue wards on a pro bono basis, but since January, she’s been a senior fellow at the Kaiser Family Foundation and editor-at-large for public health at Kaiser Health News. As part of the role, she makes regular appearances on CBS News programs. As she shifts gears and the pandemic lurches forward, her goals remain the same: to explain science, policy, and medical outcomes as clearly as possible, and to do her best to make sure that the people most at risk from the virus, including communities of color and immunocompromised people, aren’t forgotten. “The same people who get left behind are getting left behind — again,” she says. “That’s what has me really sad.”
The pandemic, like no other health crisis, has put the spotlight on these physicians due to the rapid pace of change in the virus and public health conditions, flood of data and research in need of interpretation, and demand for information to supplement official government communications.
Gounder started Princeton young — at 16 — and with a very different potential career trajectory. Her father, an engineer, “wanted me to be the next Bill Gates,” she says. He hoped she would pursue an engineering degree at Princeton, attend business school, and perhaps join him in a family business. She had different thoughts — of public service, possibly through medicine. So, in addition to her engineering course load, Gounder took premed classes, a notoriously difficult academic combination. The heavy course load didn’t leave much time for electives or exploration. “I hated the classes I was taking that weren’t of interest to me,” she says. “I saw no connection between those classes and what I was going to do with my life.” After “two years of fighting,” her father permitted her to change course and major in molecular biology.
As a junior, she took two classes that proved to be formative, one in medical anthropology — which introduced her to the work of Paul Farmer, the late medical anthropologist, physician, and founder of Partners in Health, and an advocate for addressing the root causes of global health inequalities — and another in health and human rights. She spent the summer before her senior year as an intern with the World Health Organization in Geneva and wrote her senior thesis on polio eradication and on disease-eradication programs more generally. She wasn’t 100 percent sure about becoming a doctor, but she knew she wanted to approach public health in an interdisciplinary way, pulling in anthropology, sociology, politics, and epidemiology.
After she graduated, Gounder began a fellowship through Project 55 (now Princeton AlumniCorps), working on the Tuberculosis Initiative, a treatment advocacy project initiated by Ralph Nader ’55, who had been trying to get the Clinton Administration to do more to combat the disease. “It was spreading in drug-resistant form in some countries. It was killing people — we had remedies, but people weren’t taking enough of the drugs. We had essentially eradicated it in the U.S., but it was coming back, mostly in prisons,” recalls Nader. Gounder and her classmate Scott Regenbogen ’97 reached out to members of Congress, Clinton Administration officials, and government agencies to try to get awareness of, and funding for, TB on their radar.
Gounder went to Johns Hopkins Bloomberg School of Public Health for a master’s degree in epidemiology, and along the way, studied HIV and TB in Rio de Janeiro (and later, in African countries including Malawi and South Africa). She made the decision to go to med school, she told PAW in 2018, after a colleague told her that you couldn’t really understand disease until you took care of patients. After med school at the University of Washington and an internal medicine residency at Massachusetts General Hospital, she returned to Hopkins for an infectious-disease fellowship. The public sector seemed like a natural next step, and in 2012, she took a job as the assistant commissioner and director of the Bureau of Tuberculosis Control of the New York City Department of Health and Mental Hygiene. There she ran smack into the reality of the underfunded public health system, facing budget cuts and an immediate need to let go of 20 percent of her staff. “It was just extremely demoralizing,” she says, and the scant funding made it difficult to get good work done. With more cuts projected for the years ahead, she laid herself off instead, after less than a year on the job.
Then Gounder did something totally new for her: She took a six-month break from work. She started to think, with the help of a career coach, what her next steps might be, realizing that she valued “creativity and autonomy and impact.” She recognized the role science communication had played in her career so far, from TB briefings on Capitol Hill to town halls in South Africa to meetings with activists. Her husband, Grant Wahl ’96, is a sports journalist, and Gounder realized she’d absorbed by osmosis at least something about how the business works. When she returned to medical practice, it was halftime; in the rest of her time, she began writing and making TV appearances. Her first pitch to The Atlantic — a story about medical emergencies on airplane flights — was accepted and ran in 2013.
In 2014, the Ebola pandemic raging in West Africa led to several cases in the U.S., including a New York City physician who had just returned from working in Guinea and was treated at Bellevue. Gounder remembers that when she was interviewed on TV, she was asked about convoluted scenarios through which the virus might spread in New York, even though it was scientifically established that it was transmitted through direct contact with bodily fluids and not until someone showed symptoms. She was frustrated by what she thought was shallow, misguided coverage.
“The focus wasn’t on: Why are these countries vulnerable to this? And what are the systems solutions to that?” she says. There was a lot of Western speculation, for example, on why people in Ebola-stricken areas in West Africa weren’t following instructions to refrain from burying the bodies of the dead themselves to avoid contracting the virus, and to instead wait for official response teams. But Gounder didn’t feel that U.S. reporters going to West Africa were accurately conveying the perspectives of local people. She notes that response teams were slow, which meant a family member’s body might sit for a day until it could be fetched. And when they came, they were initially using black body bags, though white is a traditional color of mourning. She realized the need for better reporting that included the people who were most at risk. “Consulting with the community really matters,” says Gounder, who volunteered as an Ebola aid worker in Guinea for two months in 2015.
After Ebola, she decided to turn her focus to health inequities in the United States. She spent several months of the year treating patients at Indian Health Service and tribal health facilities. And she decided to start a podcast highlighting the nation’s health divide. In 2017, she launched In Sickness and in Health (now American Diagnosis), which she hosts; its four seasons so far have covered youth and mental health, the opioid overdose crisis, gun violence, and Indigenous health. Dr. Mark Rosenberg, president emeritus of the Task Force for Global Health, appeared on American Diagnosis to talk about his experience using science and finding political common ground on gun violence. “She is driven by a very strong moral compass,” he says. And as a journalist, “she doesn’t approach the question with the belief that she already knows what is going on,” he says. “She understands that different disciplines and different perspectives are all important in understanding the problem.”
Gounder’s experience and proven communication skills put her back on the media’s radar when COVID hit. There have always been public-facing physicians — think of pediatrician Benjamin Spock. But electronic publishing tools such as blogging platforms and, more recently, social media, have propelled a flood of physicians into the public sphere, says Dr. Joel Topf, a nephrologist at the Oakland University William Beaumont School of Medicine in Rochester, Michigan, who is himself a public physician and has studied the phenomenon. And with COVID, there was “a huge, almost insatiable demand for information” from the public, he says.
Gounder and other physicians with the right credentials who could explain the rapid-fire developments in ways that the general public could understand were in high demand from media. Successful public health messengers on TV can deliver information “with warmth, to convey the uncertainty when there is some, and to connect with people,” says Sarah Gollust, an associate professor of health policy and management at the University of Minnesota School of Public Health. Those familiar faces have interpreted the evolving public health guidance and have explained how science works, she adds.
Regenbogen, Gounder’s Tuberculosis Initiative colleague and now a surgeon at the University of Michigan, says that Gounder, along with Brown University’s Dr. Ashish Jha (now the White House COVID response coordinator), surgeon and author Atul Gawande, and University of California, San Francisco, trauma surgeon Andre Campbell, “were the right voices that bubbled to the top” of media coverage. “In all of those cases, you’re hearing from people who have exactly the right distance. They weren’t virologists — they weren’t too deeply into it. They have provided a really broad and interesting perspective.” (Gounder also communicates via Twitter, where she has about 90,000 followers.)
“There’s a real trustworthiness to the way in which she communicates information,” says Dr. Helene Gayle, president of Spelman College, who met Gounder through her work on TB. “She is straightforward and doesn’t go beyond what is known.” Lately Gounder has written and spoken about the omicron BA.5 subvariant as well as other public health issues, including the effects of climate change on health, the medical impact of overturning Roe v. Wade, and this year’s U.S. outbreak of monkeypox. She has criticized the response to that virus, saying on CBS in late June that the country should have “ramped up education and access to testing a few weeks ago,” and that once it became clear the virus was spreading in the United States, “we should have deployed vaccines from our national strategic stockpile more quickly and broadly, not just for close contacts, but for others known to be at high risk for monkeypox.”
She speaks just as plainly about the U.S. response to COVID. Vaccine development and rollout went “really well,” Gounder says. Despite early worries about being able to ramp up enough manufacturing capacity, the first half of 2021 “was spectacular” in terms of administration, with credit going to the Trump Administration for Operation Warp Speed, a public-private partnership that funded development for some vaccines. But the pandemic has revealed the rickety infrastructure of the public health system in the United States, she says. Back in 2008, a prescient report by the Association of Schools and Programs of Public Health warned of a shortfall of 250,000 public health workers by 2020. Information systems at local public health departments are “like a flashback to the 1980s,” she says.
And the pandemic quickly became another front in the cultural and political wars that have wracked this country. Even at the beginning, calling the COVID outbreak a pandemic was seen as political. In April of that year, Gounder wrote an op-ed for CNN calling for health-care workers and scientists, not politicians, to be the key figures in communicating to the public about the pandemic. As she had seen in Guinea, where the Ebola outbreak occurred a year before a presidential election, political leaders taking center stage only reinforced suspicion and mistrust in government. In a time of intense political divisions, having then-President Trump or then-Governor of New York Andrew Cuomo as the key figures addressing the public was a mistake. “You immediately lose anyone who is from the opposing party, because of who the messenger is,” she says.
Gounder was a member of President Biden’s Transition COVID Advisory Board, which dissolved after Biden’s inauguration. Last January, she and two other members of the transition team — physician and bioethicist Ezekiel Emanuel and epidemiologist Michael Osterholm — published a viewpoint piece in the medical journal JAMA calling on President Biden to adopt a different national approach to dealing with the “new normal” of COVID. They noted that eradication is not a valid strategy, since vaccination and infection do not provide lifelong immunity and because some animals can harbor the virus.
In February, she wrote a piece for Stat News trying to make sense of where the pandemic might go next. “There’s a lot more that can be done to prevent transmission and mitigate disease without shutting down society or the economy,” she wrote.
In addition to modernizing and bolstering the public health system, they recommend considering the combined risk of major respiratory viruses, including the SARS-CoV-2 virus that causes COVID, flu, and respiratory syncytial virus (RSV). The country should adopt an “appropriate risk threshold” reflecting a certain level of death, hospitalizations, and community prevalence. When hospitalizations and deaths rise above a preset level, mitigation measures could be implemented, and hospitals could add personnel and expand capacity. The point, Gounder says, is to ask how we can reduce the overall population risk of all these viruses in a sustainable way. Just as we check the weather forecast to decide whether to bring an umbrella, we might someday check on respiratory-virus prevalence to decide whether we should wear a mask on our subway ride to work. She’s worried that the tough flu season in Australia could predict a tough flu season here — which, on top of COVID activity, could hit hospitals hard.
In a January interview with The Washington Post, she said that “our new normal should include a strategy to assume there will be at least one or two new variants per year, and to be prepared for that, so that it doesn’t take us by surprise, so that we don’t have to take draconian measures to control it, but we’re prepared to deal with it.” The fact that many people in the United States seem to be embracing not a new normal, but a 2019-style normal, and claiming they are “over” COVID, is hanging heavy on Gounder, who sees many efforts left undone even though they could mitigate the risk of COVID and the next pandemic for vulnerable communities. There’s no national paid medical and family leave, which incentivizes low-wage, public-facing service workers to clock in even when they’re sick. Funds to update HVAC systems in K-12 schools haven’t always filtered down to the schools. Government funds to pay for testing and treatments for the uninsured expired earlier this year. Gounder worries we have retreated into calculations about individual risk, rather than focusing on collective actions to protect everyone.
Many of the million-plus people who died of COVID in the United States passed away without even relatives in attendance, their family members often left to say goodbye over an iPad or phone. But in a country of 330 million, with risk of disease and bad outcomes spread unevenly, many people don’t personally know anyone who died. “For some people it isn’t something that has touched their lives except through restrictions and mitigation measures,” Gounder says. She also suspects that the characteristics of the dead have influenced how people think of the collective loss. In December, as the omicron variant was marching through the U.S. population, she wrote in The Atlantic that COVID deaths occurred mostly among the elderly, and disproportionately among Latino, Black, and Indigenous people. “We do not value the elderly. We do not value Black and brown Americans,” she wrote. “Where there is structural violence and systemic racism, infectious diseases will flourish.”
In February, she wrote a piece for Stat News trying to make sense of where the pandemic might go next. That depends on three variables — the virus, immunity, and human adaptation — and is hard to predict, she says. But she felt confident in saying, “U.S. hospitals are not ready for the new normal,” citing staffing shortages, low morale, and a still-fragmented health-care system. “There’s a lot more that can be done to prevent transmission and mitigate disease without shutting down society or the economy,” she wrote. “But I fear that we will default to business as usual, leaving it for the American health-care system to treat what could have been prevented. And, as usual, this system will do what it does best: provide care expensively, inequitably, and with underwhelming results.”
If that doesn’t sound optimistic, it’s not supposed to. Gounder and many of her fellow health-care workers are only now processing the trauma of the last two years, and they are disheartened. “There’s so much promise and potential for doing things better, and for not repeating the same mistakes next time. I don’t think we’ve learned, still,” she says. “It’s not that I think we shouldn’t peel off mitigation measures — I think it’s appropriate to be moving in that direction. But you should do so and at the same time be building in safety nets, building in ways to insulate ourselves better if there’s another surge, or another pandemic.”
Katherine Hobson ’94 is a freelance journalist focusing on health and science.






No responses yet