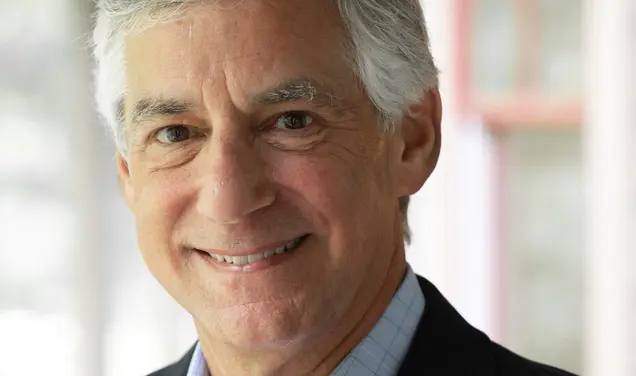
Q&A: CDC Director Rochelle Walensky Talks About Pandemic Next Steps
Rochelle Walensky, director of the Centers for Disease Control and Prevention (CDC), sat down with PAW when she visited campus March 24 for a talk with President Emerita Shirley M. Tilghman and members of the Class of 2022 as part of the seniors’ Last Lectures series. During our brief yet wide-ranging conversation, Walensky gave her take on lessons learned — often with great difficulty — from the COVID-19 pandemic, as well as potential silver linings.
The pandemic has impacted us all, and the world may never return to “normal.” How has it changed college communities specifically?
Well, certainly my heart goes out to so many college kids around the country who lost vital college time. I have several among them. So, I know. There’s such a growth opportunity that college delivers in terms of social, emotional, and academic growth. I know much of that happened, and there were a lot of opportunities to try and foster that even during the pandemic. But it’s a precious four years, and some of our kids lost some of that.
I think it also demonstrated the creativity of how people connect and can remain connected, and opportunities for how they can make lemonade out of what they lost. So, I think that it has led to innovation and ingenuity and all sorts of things in terms of connection. And I think the kids are really glad to be back.
What do you think colleges and universities should take forward as lessons learned from the pandemic?
I just had the great opportunity to tour the [University’s COVID-19 testing lab] that was set up for PCR screening. The ability for this university to be able to do that in [the fall of] 2020 and to deliver to make sure that kids could come back is truly creative, and not just creative, but scientifically the logistics behind it ... everybody came together as a community. How we leverage that lab to do other things, I think, will be incredible.
I think [the pandemic] fostered a real attention to mental health, especially for this age demographic. Certainly there have been tragedies. Many tragedies. I mean, America’s lost nearly a million people, and that is many of this generation’s family members, if not individuals.
And then, [we see] all of the other challenges in public health around it. As I look back to my own life during that period of time, it was these kinds of things — for me it was HIV and AIDS — that motivate the next generation. So, we are seeing more medical school applications, more applications to public health schools. We certainly need that talent in those fields, especially in this moment, so perhaps it will be motivating scientifically for a new generation as well.
You touched on mental health. As we come out of the pandemic, how do we not lose sight of the additional stress and accompanying ripple effects that are affecting so many people?
I think the long-term manifestations of what has happened over the last two years will be the source of many studies. We have gotten very good at counting cases of COVID and cases of hospitalizations due to COVID. We’ve gotten less good at really understanding the ancillary impacts, and certainly mental health is going to be one of them. And so, unfortunately, I think we have more to learn there. But I think we do need to make sure there are resources available, because this is going to be, I think tragically, one of the manifestations that we’re going to continue to see in our scientific study.
Burnout has also been a very real consequence. How do we move forward while dealing with so many stressors?
Thirteen thousand people at the CDC [have been] working in public health for 75 years, and yet we’ve never worked through a pandemic. We have 2,000 people in our response, and so I am feeling well the challenges of burnout within the CDC, in public health, in medicine, in health-care workers. I think that that is among the mental-health challenges of the moment. We’ve been working really hard to make sure that people check out, take the time that they need so that they can recharge. I have said we need to “tag out.” That’s what we’ve been doing in our response: making sure that people can have the family time. That it’s OK to say, “I actually need this moment, either for celebration or for mourning.” And we need to make sure that we protect one another.
The other thing that I’ve been working hard at doing is just to make people feel valued. I think people get a real recharge out of just knowing, “I see you’re working hard. And I know what you’re doing to try and achieve and go above and beyond.” Just recognizing that goes an incredibly long way. I’ve made what I call unsung-hero calls — randomly picking up the phone to people in the CDC, saying, “I heard you were the one that stayed up all night to make the flight arrangements.” People are bowled over that I’d be willing to call them and just say thank you for those efforts, but it just really goes a long way.
What other challenges has the pandemic exacerbated or raised awareness of?
Well, certainly equity. I think we in infectious disease have known that infectious diseases disproportionately impact those without resources, those in racial ethnic minority groups. We saw COVID reach our shores from people who went on airplanes and went on cruise ships, and yet it rapidly went to communities that had multigenerational households, that had many people crowding, living in a single household. And so, we have always known [that] in infectious disease, and that was laid bare during this pandemic.
If we can learn something from it, it would be to give that the extra attention that it needs. That no one is healthy until everyone is healthy. To make sure that socially vulnerable communities have access to care. That they have the resources that they need to improve their care. And that is not just in COVID, but we have seen it in maternal mortality, we’ve seen it in opioids, we’ve seen it in HIV. We seen it across the board.
Is there anything more that institutions with significant resources like Princeton could or should be doing?
I think the Princeton voice is a loud one. And I think it would be really impactful to make sure that equity is deeply rooted here in this university as well. Princeton students are so good about giving their time to volunteer in name-the-incredible-cause to make sure that the voice of equity is heard. We have been working hard to do that at CDC. And I think the important point is to do so introspectively. To make sure that there’s a diverse community within Princeton, and then to send that voice outward and make sure that those activities are bred in everything that students from here do.
Everyone wants to return to “normal.” How do we strike a balance between that desire and the health and safety of the community?
I do think that we are all yearning to get back to many of the things that we used to do and love. I think we will have a probably healthier approach of doing so. Getting back to normal — many people can’t, simply because [of] the loved ones that they lost. When I think about some of the things that I used to do that were normal — you know, I didn’t carry Purell all the time before. I bet a lot of us [will] not go out without carrying Purell. So, I think that there are many things that will be better.
I think we have seen [reduced transmission of] a lot of our respiratory viruses in the winter just by certain things that we’ve done that have protected us against coronavirus. And that’s not just masking, but respiratory hygiene and washing our hands and those kinds of things. So, there will be things that will be better because of this.
But I also think that everybody — as we have learned so much during this pandemic — everybody has their own individual risk tolerance. And that’s appropriate. It should be that risk tolerance on a college campus is different than risk tolerance in a long-term care facility. That should be the case. That’s healthy. But even within a college campus, people have their own individual risk tolerance. And so, people really have to use that as their rudder to make decisions about how I feel about going to this event and whether I’m going to wear a mask or not.
If you could look into your crystal ball, what would you say the next three to six months might look like?
My crystal ball has been really hazy in this pandemic, so it doesn’t work. I kind of need a new crystal ball.
Here’s what I think. I think we are not done yet. I think that we need to continue to be vigilant and prepared. And while everybody is sort of breathing a sigh of relief, we at CDC and [in] public health are taking this opportunity to breathe and increase our game and preparation for whatever it is that we need for whatever may come next. And that’s surveillance; that is preparing for any new variant that is out there.
What we do know is that the more [the] virus circulates, the more it has the opportunity to mutate. The more it has the opportunity to mutate, the more opportunities we’re giving for variants to emerge. And so, we are focused not only on our vigilance here, but around the world to try and get more and more people vaccinated and to build up that immunity and not give the virus more hope. In terms of the next three to six months —really the next year — if we don’t have a new variant, we will likely see fluctuations in cases. We will likely see ebbs and flows. We will likely see more disease and more deaths. And we are working now to do all the work that we can to prevent that.
Interview conducted and condensed by Julie Bonette











No responses yet