In Boston, Alumni Doctors Face COVID-19 Together
“It’s a long-term ground war,” says Edward Ryan ’84
Every day was a long day for the doctors at Massachusetts General Hospital as they waited for the surge of COVID-19 cases to hit Boston. They had been tracking the outbreak since late January, when the first cases were reported in China, but could do nothing to stop it as cases began to pop up across the United States. All they could do was plan, stock up on supplies, and brace for the worst.
Planning for the worst is Paul Biddinger ’90’s job. Biddinger is the chief of emergency preparedness and director of the Center for Disaster Medicine at Mass General, the original teaching hospital for Harvard Medical School and one of the largest hospitals in the United States, with more than 1,000 beds. Since 2015, following the Ebola outbreak, it has also been one of 10 hospitals in the country designated by the Department of Health and Human Services as a Regional Ebola and Other Special Pathogens Treatment Center. For nearly five years, Biddinger, Erica Shenoy ’98, the associate chief of Mass General’s infection-control unit, and other physicians have been war-gaming for an international pandemic, devising protocols for everything from how to keep oxygen evaporators from freezing because of overuse to the proper methods for putting on and removing personal protective equipment. (Unless otherwise indicated, all interviews were conducted during the first two weeks of April.)
No pandemic, when it comes, is exactly like the ones that had been planned for. COVID-19, Biddinger says, initially fell on the extreme end of their models, especially in terms of the degree to which it can be spread by people who show no obvious symptoms. Since January, he and Shenoy have found their days filled with a seemingly endless stream of meetings — virtual, of course — with doctors at Mass General and Partners HealthCare, the consortium of hospitals, clinics, and health-care providers of which Mass General is a part. (Biddinger also serves on the governor’s coronavirus task force, advising hospitals around Massachusetts.)
“Literally every minute is accounted for,” he says, trying to respond to incoming texts and emails while he talks. “It can be a 12, 14, 16, 18-hour day before you go home.”
Much of their time has been spent making sure the hospitals don’t run out of supplies. Do they have enough masks? Swabs? Ventilators? Testing kits? Notes Charles Morris ’92, associate chief medical officer at Brigham & Women’s Hospital, which is also part of Partners HealthCare: “A huge portion of the day is focused on the supply chain.”
Shortages continued to pop up, forcing Shenoy to rethink protocols for conserving supplies such as disposable gowns. Mass General began working with Battelle, a nonprofit based in Ohio, to decontaminate N95 respirator masks using concentrated hydrogen peroxide gas so they can be used again. Battelle opened a decontamination unit with the capacity to sterilize 80,000 masks a day in an empty former Kmart store in nearby Somerville.
COVID-19 has transformed every part of Mass General, as it has many other hospitals around the United States. There are fewer cases than usual in the emergency room, says David Brown ’85, chief of Mass General’s department of emergency medicine, but the patients are sicker. Normally they would admit about 25 percent of ER patients; now they were admitting 40 percent, and many of them were going to the intensive-care unit. Normally doctors would see two or three patients a day who were so ill they needed to be put on ventilators. In mid-April they were seeing six to 10 each day.
Necessity being the mother of invention, the hospital began using personal protective booths called “hexapods” for screening patients in the ER. A doctor stands inside a plexiglass booth and administers nasal swab tests to patients, working through gloved portholes. The booths have negative air flow, so physicians can work without wearing full protective equipment, which also helps conserve those supplies for other cases.
Mass General had to remain a functioning hospital for everyone even as it dealt with the surge of COVID patients. As Brown notes, emergencies don’t take a vacation just because there’s a pandemic. “Heart attacks and strokes and trauma and sepsis all require evaluation, investigation, and time-sensitive treatment,” he says. “We have to be able to take care of those patients, too.” But someone coming in with a broken arm might also have COVID, which if undiagnosed could infect everyone else in the unit. For that reason, everyone in the hospital, patients and staff, wears a protective mask at all times.
Visitors have been barred from the hospital, and all non-essential business has been diverted elsewhere. In the obstetrics department, phone calls or virtual visits substitute for in-person visits. The department began sending blood-pressure cuffs to pregnant women so they could take their blood pressure at home rather than having it checked at the hospital. “We have very quickly redesigned what prenatal care looks like,” says Jeffrey Ecker ’84, chief of the department of obstetrics and gynecology. New cycles of in vitro fertilization were also deferred in most cases.
“In emergency medicine, we signed up for this a long time ago with the expectation that we would be the first wave on the beach.”
— David Brown ’85
Perhaps the most important variable in managing the outbreak is testing. “We have to know who has COVID and who doesn’t,” Biddinger explains. “If we can’t get test results back quickly, that’s a huge problem.” Fortunately, the turnaround rate improved considerably, from as long as five days back in February to fewer than 12 hours in some cases to as little as two hours by the end of April, which is critical because it enables hospital administrators to determine who may safely come to work. “If we can test people and get the result back right away, we have a better chance of avoiding a staff shortage that would affect our ability to take care of patients,” Biddinger says.
Biddinger credited physical distancing with helping to “flatten the curve,” which had enabled the hospital to avoid the worst-case scenario he and others had feared. Even so, he notes, Mass General had to open four new ICU spaces around the hospital to handle the overflow of people on ventilators.
The alumni doctors at Mass General are not sanguine about when life will return to something approaching normal, either in Boston or around the country.
“It will take months to trend down from the peak,” Biddinger predicts. “Folks who are critically ill in the ICU stay critically ill for longer than other patients. It’s going to take a while for the health-care system to even vaguely get back to normal, and it will take a lot longer than that for people to feel back to normal. We’re all starting to treat each other differently, we’re all staying six feet away from each other, we’re all treating each other as potential sources of infection. Recreating those human bonds is going to be really hard.”
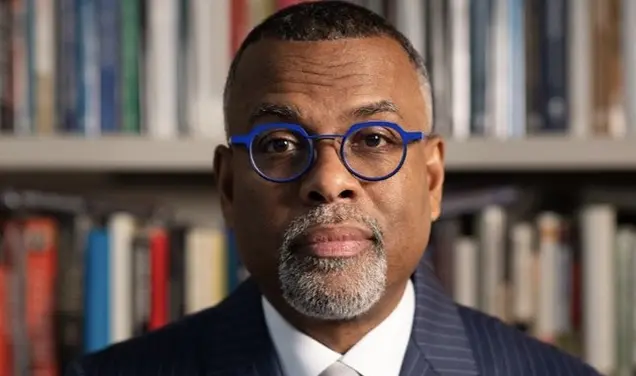
Edward Ryan ’84, Mass General’s director of global infectious diseases, is blunt in his assessment that this could be a one- to two-year process. “It’s a long-term ground war; it’s not like hunkering down for a hurricane,” he says. “Even if we get through this first wave, there is a reasonable chance that the virus will come back in August or September. So how do we unwind our social distancing? If we just send everyone back to work, the number of infections will probably flare again.”
In addition to his other work, Ryan directs a research laboratory at Mass General that focuses on infectious diseases such as COVID-19. Like others around the world, these researchers are working full time to develop a vaccine, but Ryan cautions that we are still many months away from having one that could be deployed on a large scale.
“There are only two end games here,” he says, assessing the immediate future. “One is that we let the virus sweep the planet repeatedly until everyone who survives is immune. Obviously that has a lot of disadvantages, but it is basically what we did in the influenza outbreak in 1918. The other end game is to shortcut it by developing a vaccine and deploy that in nine to 18 months. In this current wave, only 5 to 10 percent of the United States is probably going to get infected. So 90 to 95 percent of people will still be at risk after this wave passes. This [virus] is a nasty beast.”
In other words, the physicians have more long days ahead. It might seem hard to keep from burning out, but Brown sees things differently. “In emergency medicine, we signed up for this a long time ago with the expectation that we would be the first wave on the beach,” he says. “I certainly consider it the honor and privilege of a career to work in a department that can serve our patients and our community at a time like this.”
Mark F. Bernstein ’83 is PAW’s senior writer.










No responses yet