Progress to HIV Response in South Africa Fades with U.S. Aid Cuts
The country — home to an estimated 8 million people living with the virus — had been finding success through research, programming, and community activism
Five weeks after graduating from Princeton in 2013, I found myself in the backseat of a four-wheel drive, narrowly evading livestock and potholes en route to the small rural village of Zithulele in South Africa’s Eastern Cape province. Over the next year, as part of a ReachOut Fellowship, I was on a team that followed 480 mothers and their infants for the first year of life. We regularly spoke with mothers in their homes — asking questions about the household, infant feeding practices, immunizations, child development, and health care access. As we came to better understand the barriers to health care access, I learned that maternal and infant health in South Africa was inextricably linked with the HIV epidemic.

At that time, HIV prevalence was nearly 30% nationally among pregnant women, and everywhere from hospital waiting rooms to advertisements papered onto the walls of local shops contained public messaging about HIV prevention, testing, and care. Yet conversations about HIV were punctuated by hopefulness, a sense of a turning tide. Antiretroviral medication was largely available, even in the most remote pockets of the country, and widespread infant prophylaxis and testing meant that most babies were being born HIV-free.
In the past decade, this sense of momentum — in moving toward a foreseeable end to the HIV/AIDS epidemic — has continued to be a driving force in South Africa for research, programming, and community activism. It has also shaped the work I continue to do, as a South Africa-based researcher focusing on the mental health and well-being of adolescents. U.S. government investments in a wide range of initiatives and research consortia, through the President’s Emergency Plan for AIDS Relief (PEPFAR), the Global Fund to Fight AIDS, Tuberculosis, and Malaria, and the National Institutes of Health, established foundations for this remarkable progress.
However, recent changes have brought this success story to a grinding halt. It is hard to keep track of what kinds of government funding cuts have been passed, paused, and reversed in recent months. National governments of countries that long received this aid have begun to plan for the future with fewer resources. Meanwhile, the uncertainty and upheaval from cuts to date have had powerful impacts in the places, and among the people, hardest hit by the HIV epidemic. While South Africa is officially an upper-middle-income country and relies less on foreign aid than many of its neighbors, it is still home to an estimated 8 million people living with HIV.
Adolescent mothers living with HIV face distinct challenges in this moment. All young mothers experience biological, psychological, social, and identity shifts. Caring for a new infant, all while managing the ups and downs of adolescence, becomes harder as they also try to manage a chronic disease that continues to be heavily stigmatized. These factors often converge, affecting young mothers’ mental health and ability to navigate changes. These cases are not isolated, either. In the Eastern Cape, new cases of HIV are highest among young women ages 16-21, and 17% of babies are born to adolescent mothers.
In the study I have been leading in the Eastern Cape since 2023, some participating young mothers were born with HIV, and have experienced years of pill-taking by the time they turn 18. Others talk about finding out that they were several weeks pregnant on the same day they received their HIV diagnosis. One participant spoke about the shift that happened after she learned she was living with HIV: “My life changed; things were not the same as before, so I had to live a different life. This life is not normal, because I’m surviving on pills. Every morning, I must take a pill at 8 a.m., I have this burden that I must take care of,” she said, her identity protected because of privacy concerns.
While journeys in HIV care can vary, evidence shows that this burden is made lighter by adolescent-friendly health services, peer-based programming, and psychosocial support. Beyond simply getting to a health facility and leaving with pills in hand, being treated with kindness and respect can be the deciding factor in keeping young people engaged in life-saving health care. While this equation sounds simple, it is often complicated by overburdened nurses, crowded clinics, and perceptions of stigma that so many young people, especially young mothers, experience.
These challenges will only increase in the aftermath of U.S. funding cuts. With shrinking health budgets, psychological, social, and structural support is often seen as secondary — though decades of research show us that medication alone will not end the HIV epidemic. These cascading effects on HIV prevention, treatment, and retention also extend to health workers themselves, many thousands of whom were in positions funded by partners and subsidiaries of USAID and PEPFAR and have lost their jobs. The loss of key relationships, as well as human capital, deals another blow to the structures that have been successfully addressing the epidemic.
As the national government plots a way forward (too slowly, for some), these cuts continue to reverberate across different levels. For young women facing multiple layers of disadvantage — based on their gender, their HIV status, their rurality, and their identity as mothers — the actual and potential repercussions are undoubtedly greater. Still, after three decades, South Africa’s story of the HIV epidemic continues to be written with optimism and a sense of purpose.
Another young mother shared her advice after a group workshop: “What do you tell moms moving forward, from what we have talked about? Self-assurance. There is nothing as important as knowing yourself. There is nothing as important as knowing what you want to be in five years to come.”
In the years to come, addressing the HIV epidemic will require a new type of resolve, and a new roadmap, for the diverse global coalition that once mobilized so effectively in the name of a greater cause.
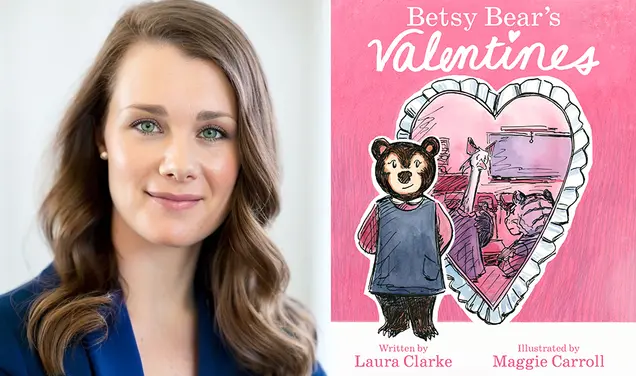
Christina Laurenzi ’13 is a Senior Researcher at the Institute for Life Course Health Research, Stellenbosch University, South Africa. In her work, she focuses on strategies to support adolescent mental health and wellbeing in contexts of adversity.











No responses yet